Why do patients stick with expensive medications when cheaper, equally effective options exist? Why do some people never fill their prescriptions-even when they know it could save their life? The answer isn’t about ignorance or laziness. It’s about behavioral economics.
People Don’t Make Rational Drug Decisions
Traditional economics assumes people act like robots: they compare prices, weigh risks, and pick the best option. But real people? They’re messy. They’re scared. They’re influenced by how things are presented, what their friends say, and even how a pill looks. A 2022 study found that 68% of patients keep taking their current medication-even when a similar one costs 30% less. Why? Fear. Loss aversion. The idea that switching might mean losing something they already have, even if it’s not actually better. This isn’t irrational in the sense of being stupid. It’s human. Behavioral economics doesn’t blame patients. It explains why they act this way. And once you understand the patterns, you can design better systems to help them.The Big Psychological Triggers
Several mental shortcuts drive drug choices. Here are the big ones:- Loss aversion: Losing something feels worse than gaining something good. Patients don’t want to lose their current routine, even if it’s expensive. A 2021 trial showed that framing a reminder as “Don’t lose your streak!” boosted adherence by nearly 20% compared to a neutral message like “Take your pill.”
- Present bias: We want rewards now, not later. That’s why 33% of prescriptions go unfilled. The benefit of taking blood pressure meds? It’s invisible. The cost? A co-pay today. The brain picks the immediate pain.
- Confirmation bias: If you believe expensive = better, you’ll ignore evidence that a generic works just as well. A 2022 analysis showed drug prices rose 47% faster than inflation-yet many patients still assume higher cost means higher quality.
- Defaults matter: When doctors’ electronic systems automatically suggest a brand-name drug, that’s what gets prescribed. One 2012 study found that simply changing the default option in prescribing software increased appropriate substitutions by 38% during drug shortages.
- Social norms: People follow the crowd. In one HIV clinic, posting public adherence rates on a wall improved patient compliance by 22.3%. No lectures. No penalties. Just showing people what others were doing.
Why Education Alone Fails
You’d think telling patients “Take your meds!” would work. But studies show traditional patient education only improves adherence by 5-8%. That’s barely better than doing nothing. Why? Because knowledge doesn’t change behavior. You can explain to someone that statins reduce heart attacks by 30%, but if they’re afraid of side effects or think the pills are too much hassle, they’ll still skip them. Behavioral economics flips the script. Instead of trying to convince people, it changes the environment to make the right choice easier. That’s the power of a “nudge.”Real-World Nudges That Work
Here’s what’s actually working in clinics and pharmacies today:- Rebate systems: A 2021 NEJM study gave patients cash back for taking their statins. Those who received $10 monthly rewards for perfect adherence had 23.8% higher persistence than those who didn’t.
- Simplified dosing: Patients on five or more medications have adherence rates 23.7% lower than those on one. Reducing pill burden-even just switching from twice-daily to once-daily-makes a huge difference.
- SMS reminders with emotional framing: “Your heart needs you today” outperforms “Take your medication.”
- Default substitutions: During a shortage, if the system auto-suggests a generic alternative, doctors are far more likely to pick it.
- Smart pill bottles: These track when pills are taken and send alerts. They improve adherence by 24.3%, but cost $47.50 per patient per month. Simple SMS texts cost $8.25.
Who Benefits Most-and Who Doesn’t
Not all patients respond the same way. Behavioral nudges work best when:- The condition is chronic (like diabetes or high blood pressure)
- There are clear alternatives (like generics)
- The patient doesn’t have severe mental health issues
- Oncology: Treatment is complex, side effects are brutal, and options are limited. Only 12.3% of oncology programs use behavioral tools.
- Depression or anxiety: Patients with these conditions are 31.4% less likely to respond to nudges. Their cognitive load is already overloaded.
- Asymptomatic conditions: If you don’t feel sick, you don’t feel the need to take pills. Adherence drops 32.7% compared to symptomatic diseases.
The Cost of Non-Adherence
Skipping meds isn’t just bad for patients-it’s expensive for everyone. In the U.S. alone, medication non-adherence costs the healthcare system $289 billion a year and leads to 125,000 preventable deaths. That’s why payers, hospitals, and drug companies are investing. The behavioral economics consulting market for healthcare grew from $187 million in 2018 to $432 million in 2022. Pharmaceutical companies make up nearly 60% of those clients. Insurance plans now have to include at least two behavioral interventions for high-risk patients under 2023 Medicare Part D rules. That’s not a suggestion-it’s a requirement.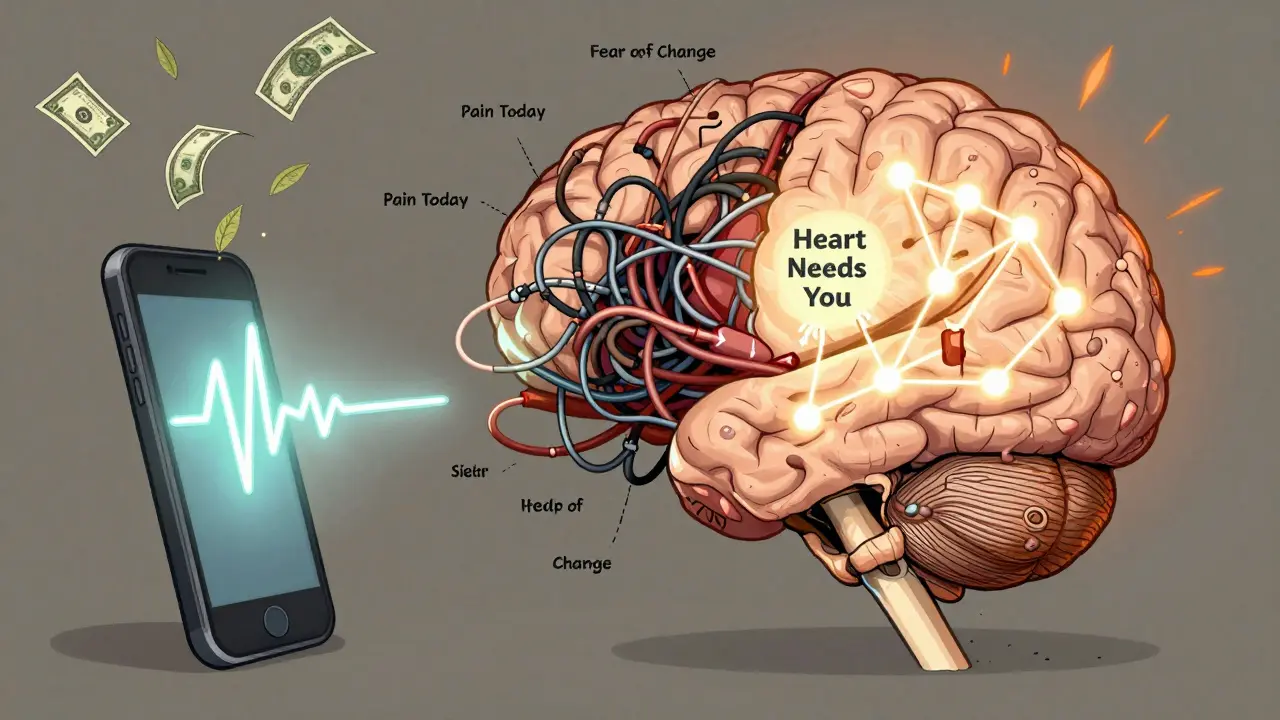
What’s Next?
The future of patient drug choices isn’t about more pamphlets or louder warnings. It’s about smarter systems:- Digital therapeutics: Apps that send personalized nudges based on your schedule, mood, and past behavior. This market is expected to grow 300% by 2026.
- AI-driven predictions: Machine learning models are being trained to guess which patients will respond to which nudges-based on age, income, diagnosis, even social media patterns.
- Value-based insurance: More insurers are tying co-pays to adherence. Lower your co-pay if you take your meds. Raise it if you don’t.
- Biosimilar adoption: Behavioral nudges have increased switching from brand-name biologics to cheaper biosimilars by nearly 30%.
It’s Not About Controlling Patients
Some critics say behavioral nudges are manipulative. But here’s the truth: every prescription form, every pharmacy layout, every doctor’s recommendation is already shaping choices. The question isn’t whether to nudge-it’s whether to nudge well. Behavioral economics doesn’t force anyone. It doesn’t take away freedom. It just makes the right choice easier. If a patient wants to skip their meds? They still can. But now, the system gives them a better chance to do the right thing.Bottom Line
Patients aren’t broken. The system is. We’ve spent decades blaming people for not taking their pills. But the real problem? We designed a system that ignores how people actually think. Behavioral economics isn’t magic. It’s just common sense wrapped in science. Understand fear. Respect habit. Reduce complexity. Use defaults wisely. Frame messages with care. When you do that, adherence improves. Costs drop. Lives get saved.Why do patients stick with expensive drugs even when generics are available?
Patients often stick with expensive drugs due to psychological biases like loss aversion (fear of losing what they’re used to), confirmation bias (believing higher cost means better quality), and present bias (focusing on immediate hassle over long-term benefits). Even when generics are equally effective, the emotional comfort of staying with a known brand outweighs the financial savings for many.
Can simple reminders improve medication adherence?
Yes-but not all reminders are equal. Neutral messages like “Take your medication” have little effect. Messages framed around loss aversion, like “Don’t lose your streak!” or “Your heart needs you today,” improve adherence by up to 20%. The emotional tone matters more than the frequency.
Do behavioral interventions work for everyone?
No. They work best for patients with chronic conditions like diabetes or hypertension who have clear treatment alternatives. They’re less effective for people with severe mental health conditions, complex regimens (like cancer treatment), or asymptomatic diseases where symptoms don’t remind them to take pills.
What’s the difference between behavioral economics and patient education?
Patient education tries to change knowledge. Behavioral economics changes the environment to make the right choice easier. Education improves adherence by 5-8%. Behavioral nudges like defaults, rebates, and social norms improve it by 20-30%-and often with less effort.
Are behavioral nudges ethical?
Yes-if they preserve choice. Behavioral nudges don’t force anyone. They make the healthier option more visible or easier to pick. A doctor can still override a default. A patient can still skip a reminder. The goal isn’t control-it’s support. Ethical nudges respect autonomy while reducing friction.
How much do behavioral interventions cost?
Costs vary. Basic SMS reminders cost about $8.25 per patient per month. Smart pill bottles with tracking cost $47.50. Cash rebate programs cost more upfront but reduce hospitalizations, saving money long-term. Most programs pay for themselves within a year by cutting avoidable ER visits and complications.
Is behavioral economics used in the UK healthcare system?
Yes, but slowly. The NHS has piloted behavioral interventions in diabetes and hypertension programs, especially around prescription refill reminders and simplifying dosing schedules. However, adoption is uneven. Academic medical centers use it more than community clinics. Funding and staff training remain barriers.
Can I use behavioral economics to help a family member take their meds?
Absolutely. Start small: simplify the pill routine if possible. Use a pill organizer with alarms. Frame reminders positively: “You’ve taken your meds for 10 days straight-keep going!” Avoid guilt. Celebrate consistency. If they’re on multiple meds, talk to their doctor about switching to once-daily options. Small changes, done right, make a big difference.





Vu L
December 27, 2025 AT 23:49Bro, this whole post is just corporate jargon dressed up as psychology. People don’t take meds because they’re broke or the system’s rigged-not because they’re ‘present biased.’
James Hilton
December 28, 2025 AT 11:11So you’re telling me a text that says ‘Your heart needs you today’ works better than ‘Take your pill’? 😂 I’d rather die than get a motivational text from my pharmacist.
Debra Cagwin
December 28, 2025 AT 20:08This is actually one of the most compassionate takes on healthcare I’ve seen in a while. So many people blame patients for non-adherence, but the truth is-our systems are designed to fail them. Simplifying dosing, using positive framing, reducing cost barriers-these aren’t ‘nudges,’ they’re basic human decency. Thank you for writing this.
Celia McTighe
December 29, 2025 AT 00:37OMG YES. I had my grandma on 7 meds and we switched to a pill organizer + weekly text that said ‘Proud of you for taking your heart pills!’ 🥹 She hasn’t missed one in 6 months. It’s not magic-it’s love wrapped in a reminder.
Teresa Marzo Lostalé
December 29, 2025 AT 03:50It’s funny how we call it ‘behavioral economics’ like it’s some new science. Humans have always made decisions based on fear, habit, and social pressure. We just finally gave it a fancy name so consultants could charge $300/hour to tell doctors to stop auto-filling brand names.
Hakim Bachiri
December 29, 2025 AT 23:10Let’s be real-this is all just a Trojan horse for Big Pharma to push generics under the guise of ‘nudging.’ They’ve been lobbying for this for years. And now they’re getting paid by Medicare to ‘help’ us… while still jacking up prices on the drugs they don’t want us to switch from. 🤡
ANA MARIE VALENZUELA
December 30, 2025 AT 08:17Wow. Just… wow. You spent 2,000 words explaining that people are emotional creatures? Did you need a $432M consulting industry to figure this out? The real scandal is that we’re still treating patients like rational robots in 2025. Pathetic.
Ryan Touhill
December 30, 2025 AT 23:20While the behavioral economics framework is undeniably insightful, it remains fundamentally incomplete without addressing the structural inequities that underpin medication access. The notion that a $8.25 SMS can compensate for decades of underfunded primary care, racial disparities in prescribing, and pharmaceutical monopolies is not just reductive-it’s morally negligent. Nudges are not policy. They are Band-Aids on bullet wounds. The real intervention? Universal healthcare. Guaranteed prescriptions. Eliminating co-pays. Until then, we are merely optimizing the machinery of exploitation.
Let us not confuse behavioral refinement with systemic justice. The fact that a patient’s adherence improves when framed as ‘Don’t lose your streak!’ speaks less to human psychology and more to the tragic absence of dignity in our medical infrastructure.
And yes-I do find it ironic that the same institutions that profit from non-adherence are now the primary funders of these ‘solutions.’ The market doesn’t fix failure; it monetizes it.
So while I applaud the nuance of the research, I implore us to stop celebrating the aesthetics of intervention while ignoring the architecture of harm. We need structural reform, not behavioral choreography.
And to those who say, ‘But it saves lives!’-yes, it does. But so would a $500,000 investment in community health workers. Why are we funding texts instead of people?
This isn’t about nudging patients. It’s about finally nudging power.