The feeling of a chest stuffed up with stubborn mucus is something you don’t forget – your breathing starts sounding like an old radiator, your cough gets raspier, and sleep’s just a distant memory. You try everything from hot showers to lemon-honey teas, yet sometimes the gunk won’t budge. Here’s a little-known but surprisingly reliable trick: chest percussion. It's not fancy, but when you need to break up chest congestion, this simple tapping technique has offered relief for decades – not just at home, but also in hospitals and physiotherapy clinics across the world.
Why Chest Percussion Works: The Science Behind the Hands
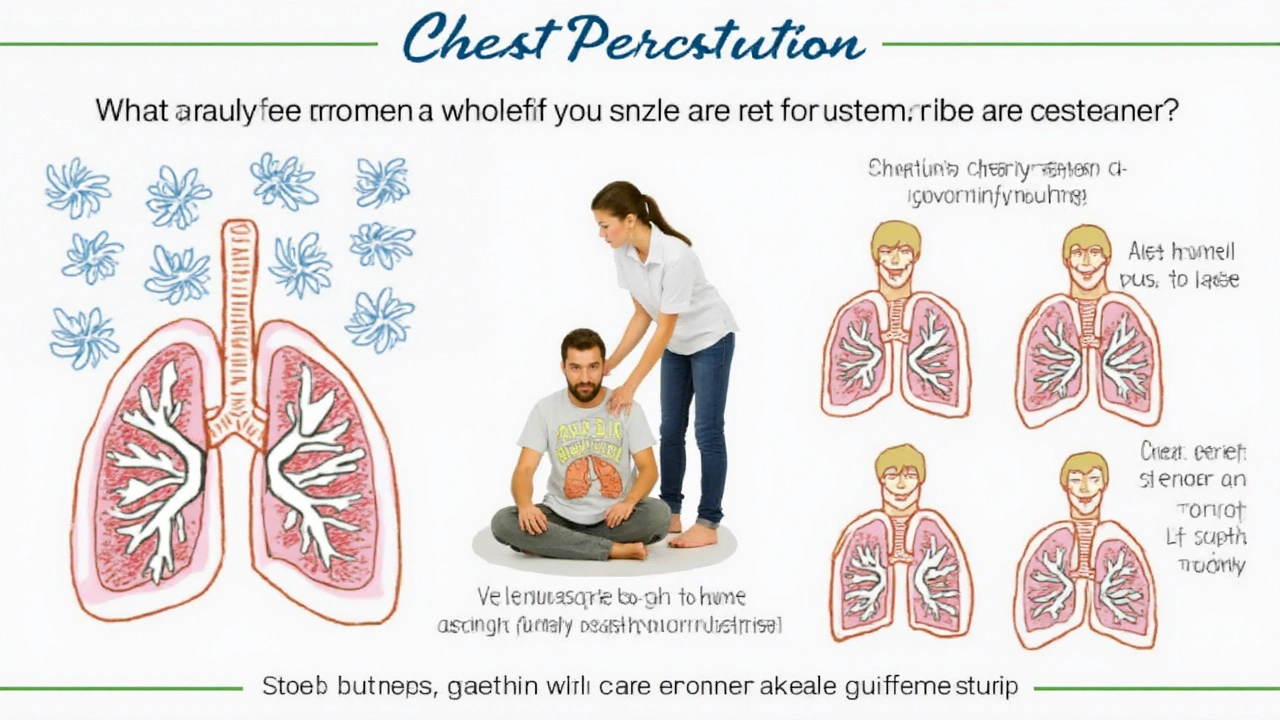
When you look at all the stuff lungs do day in and day out, clearing out mucus should be a breeze. But let’s be real–when illness hits, your natural defenses, like cilia (tiny little hairs moving mucus out like conveyor belts), can lag or even stop. Enter chest percussion, a technique where rhythmic clapping or tapping on the chest loosens up mucus deep in the lungs. It's sometimes called chest physiotherapy (CPT) and it's used in hospitals for everything from severe asthma to cystic fibrosis and pneumonia, especially in kids and folks with chronic conditions.
The trick lies in the vibrations. By rhythmically tapping on specific parts of your chest and back, you help break up thick mucus clinging to the airways. The loosened mucus moves closer to the larger airways, making it easier to cough up and finally breathe clearer.
“But Ewan, does it really make that much difference?” you might wonder. Genuine evidence says yes. For people with cystic fibrosis, a rare but tough genetic lung condition, chest percussion is a lifeline—it can cut the risk of serious lung infections and help keep airways clear. There’s a solid clinical trial from 2022 that found chest percussion reduced the length and severity of hospital stays for children with severe pneumonia by nearly 27% compared to just regular care. Even if you’ve got a nagging chest cold, this technique can sometimes help when everything else feels useless.
It's surprisingly common in the UK, especially in respiratory wards and children’s hospitals. Nurses and physios are taught the right patterns and spots, and there’s even special equipment–from hand-held cups that mimic the percussive motion, to vibrating vests for people who need daily treatments.
But you don’t always need fancy gadgets: with some guidance from a nurse or physio, this can be done at home, especially if you look after someone with a long-term chest condition. The key is hitting the correct areas for the right amount of time and always keeping things safe.
Just to be precise, chest percussion isn’t the same thing as a pat on the back or a thump on the chest. The rhythm, position, and pressure all matter, and done wrong, you could end up sore or even risk bruising.
Practical Tips: How To Do Chest Percussion Safely and Effectively
So, how do you actually do chest percussion at home without needing a medical degree or accidentally hurting someone? It’s not rocket science but there’s definitely a right way and a wrong way. I’ve talked to respiratory therapists from Liverpool’s own Alder Hey Children’s Hospital, and they give some golden advice for home sessions.
chest percussion must be done with a cupped hand—imagine you’re scooping water and keeping your fingers together, not flat or stiff like a slap. The technique involves gentle but rhythmic clapping against certain areas of your chest or back where the lungs are closest to the body surface. For adults, the most common area is between the shoulder blades, just below the collarbone, or on the sides of the chest. For children or infants, always check with a GP or respiratory nurse first.
- Find a comfortable place to sit up or lie down with support. Some people prefer lying on their front or side, propped up with pillows.
- Always use a towel or layer of clothing over the skin to cushion the impact and protect delicate skin.
- Make your hand into a soft cup. Clap in a rhythmic, drum-like motion—like a gentle drumming, not slapping.
- Move your hand in a circular motion over the chest sections, keeping a steady rhythm for 3-5 minutes per area.
- Encourage the person to cough every so often to clear any loosened mucus. A glass of water and tissues nearby help.
Never do chest percussion over bare skin, bones (like the spine or breastbone), wounds, or anywhere bruised. Avoid tummy areas in newborns and young kids. If you notice pain, wheezing that worsens, bloody mucus, or someone looks distressed, stop right away–that’s time to check in with a doctor.
A few handy things make it comfier: use pillows to get the body at a slight angle (the head lower than the chest if the doctor says it’s okay—this postural drainage lets gravity help). After percussion, always sit up, cough, and spit out any mucus loosened. It sounds clinical, but once you’ve seen the difference with someone struggling to breathe, you’ll know it can be genuinely life-changing.
Here’s a quick look at the steps and safety notes in a table:
| Step | What To Do | Why It Matters |
|---|---|---|
| 1 | Position the person lying with chest accessible, head slightly lower | Gravity helps mucus drain easier |
| 2 | Use a towel over skin | Prevents irritation or bruising |
| 3 | Cup your hand | Creates a vacuum effect without causing pain |
| 4 | Percuss over correct lung regions, avoid bones and wounds | Targets mucus, reduces injury risk |
| 5 | Encourage deep breaths and regular coughing | Clears loosened mucus from airways |
| 6 | Monitor for pain or distress; stop if either happens | Keeps it safe for everyone |
Who Benefits Most: Real-World Stories and Evidence
Chest percussion isn’t just something out of an old-school medical book. In fact, talk to anyone with a chronic lung condition, like bronchiectasis, cystic fibrosis, or even stubborn bronchitis, and you’ll hear plenty of stories about how this simple trick made daily breathing possible.
Take kids with cystic fibrosis across the UK. Their lungs produce extra-thick mucus that can block airways and attract bacteria. These kids often do chest percussion at home two to three times a day with their parents or carers. It’s not always fun, but most families swear by the way it keeps lungs clear and infections at bay. A 2023 NHS survey from Liverpool hospitals found that nearly 85% of patients using regular chest percussion (alongside inhaled meds and airway clearing exercises) had fewer emergency hospital visits over 12 months.
For older adults or anyone recovering from chest infections, chest percussion can also help shift leftover gunk that lingers even after you feel “better.” It’s common practice after certain surgeries (like heart operations) to get patients coughing up trapped mucus and prevent pneumonia. Hospitals train respiratory physios in the right technique to avoid injury and make the sessions as comfortable – and effective – as possible.
If you’re dealing with a cold that’s moved to your chest, asthma with extra gunk, or a lingering cough after flu, ask your GP or practice nurse if chest percussion is safe and helpful for you. Remember, this doesn’t replace medications, inhalers, or antibiotics when you need them – but it can be a bonus tool to clear things out naturally. In home-care settings, older people struggling to cough or clear their lungs after a long stay in bed may also benefit from gentle, regular percussion therapy.
Of course, not everyone should use this technique. People with broken ribs, osteoporosis, very low platelets, or blood clotting disorders should skip percussion, because it risks injury or bleeding. If you’re ever unsure, a chat with your GP or a respiratory nurse helps clear things up.
Beyond the Basics: Making Chest Percussion Part of Your Routine
Sometimes it’s the simple things that stick. Chest percussion isn’t glamorous, but if you’re managing a lingering chesty illness, it can be a staple part of the daily routine, just like brushing your teeth. It’s usually best to do it after inhalers, nebulisers, or steam (when the mucus is thinnest) and before meals, so coughing doesn’t upset your stomach.
Families that do chest percussion say it turns into bonding time – surprisingly, some little ones even think the drumming feels comforting or ticklish! For solo adults, if you can’t reach your own back or sides, booking a session with a respiratory physio or a trained home care worker helps keep things on track.
You don’t need fancy oils, expensive tools, or miracle chest balms. As long as you work with the right areas, stick to a soft, steady rhythm, and keep things safe, this hands-on approach works. If you use percussion regularly, keep an eye out for changes: more gunk than usual, pain, or any strange symptoms mean it’s time to check back in with a health pro.
Small steps count for a lot. Simple routines—chest percussion, good hydration, deep-breathing exercises, and using prescribed meds—can transform how you handle chest congestion, especially in people who seem to always have a cough no matter the weather.
Last tip: Don’t be embarrassed to ask your nurse for a quick demo – these folks have endless patience and can show you the cupping rhythm or correct hand shape way better than a YouTube video ever could. Once it clicks, the difference in your breathing after a session really does speak for itself.




Pramod Hingmang
July 18, 2025 AT 00:15Chest percussion—now there’s a technique that truly shows how hands-on therapy can be surprisingly effective. I love how this method isn’t just about force but carefully timed taps to loosen mucus. It’s like giving your lungs a gentle wake-up call!
What stands out to me is how rooted it is in respiratory therapy, not just some home remedy passed down as folklore. Plus, the fact that it helps mucus clearance fast means it could really change the misery levels during congestion.
However, I’m curious about the dos and don'ts—are there any risks if done incorrectly? I’ve always heard you shouldn’t just start tapping randomly without some guidance. Anyone with experience here?
Richa Ajrekar
July 18, 2025 AT 01:23Honestly, I don’t get the fuss about chest percussion. It’s yet another method hyped without proper clarity. Many articles like these often forget to mention that improper technique can injure ribs or cause more discomfort. Also, what about those with underlying conditions? Is it safe for everyone?
And why do people continue with this outdated practice when modern medicine offers inhalers or nebulizers that are scientifically proven? If someone really wants to clear airways, turn to actual medicine, not slapping your chest. It feels like common sense being ignored.
Also, grammar-wise, your article needs tightening up. If you’re aiming for professionalism, don’t undermine it with sloppy sentences.
Virat Mishra
July 18, 2025 AT 11:13Oh come on, Richa, don’t be such a downer. There’s nothing wrong with good traditional methods, especially when they work. Sometimes the old ways are just as valid as new tech. And seriously, if a gentle tap on your chest can ease you up, why not give it a shot?
People overcomplicate these things. They hear 'outdated' and run away when maybe they just haven’t tried it or understood the process fully. I mean, coughing alone doesn’t do enough sometimes, so percussion might be the magic touch.
Still, I get the safety concerns. Not something to do with reckless energy.
Daisy Aguirre
July 19, 2025 AT 22:58This article is a lovely reminder that sometimes simple techniques have a place in modern care. Chest percussion provides an accessible option for many, especially those who can’t easily get to medical facilities or afford costly treatments.
I think highlighting practical tips and emphasizing correct techniques is crucial so people don’t hurt themselves. It’s all about just being gentle yet effective.
And yes, mucus clearance is no joke. When your airways are blocked, it’s like breathing through a tunnel — anything to open them up eases so much suffering. Proud to see cultural practices being respected even in medical circles.
Natalie Kelly
July 20, 2025 AT 22:08This sounds pretty useful, especially for people who have chronic bronchitis or other conditions that produce stubborn mucus. The dos and don'ts part seems important though — it’d be great if the article provided some video tutorials or visual aids.
I know a few folks who’ve tried chest percussion and said it really helped them breathe easier, but they were taught properly by a respiratory therapist first. Randomly trying it yourself might backfire.
Does anyone know if children or elderly people can safely get this done at home? I’m wondering if there are age restrictions or precautions.
Tiffany Clarke
July 22, 2025 AT 00:05Ugh. This article makes it sound so easy but I can’t stand the idea of slapping my chest. The sound alone would make me cringe. And what if it just spreads the germs more? Feels kinda gross.
Plus, I’m all for natural stuff but sometimes you gotta just take meds and chill. Why complicate with manual stuff that might stress you out more? Just my two cents.
Anyway, grateful for the info but I think I’ll let the pros handle this one.
Sandy Gold
July 22, 2025 AT 22:28Actually, the historical context of chest percussion dates back much further than most assume. It was first formalized in the late 19th century by respiratory therapists who wanted to improve mucociliary clearance specifically. To dismiss it as 'old-school' without recognizing its clinical foundations is rather short-sighted.
Moreover, not everyone who is congested needs inhalers or nebulizers—they're not always accessible or appropriate. Chest percussion is a low-tech adjunct that, when done thoughtfully, contributes significantly to airway hygiene.
I do agree that the article could improve in grammar and structure, but content-wise it’s solid and informative.
Frank Pennetti
July 24, 2025 AT 00:20From a clinical perspective, chest percussion involves targeted mechanical stimulation of the thoracic cavity to mobilize pulmonary secretions. It activates the mucociliary escalator facilitating expectoration. Scientifically, the evidence is a mix—but in many tertiary care settings, it's still recommended for particular patients.
There are vital precautions, though. Over-percussion can potentially fracture ribs or cause pleural irritation. Plus, it's contraindicated in cases like osteoporosis or recent chest trauma. So, a risk-benefit analysis is essential before starting this.
Despite being less flashy than inhalation therapy, it remains a viable adjunct in respiratory care, especially when devices aren't available.
Adam Baxter
July 25, 2025 AT 01:10That's awesome info! Gotta keep the airways clear bro, breathing right is #1. Chest percussion might sound old school but it still packs a punch. Sometimes nature’s simple solutions rock the hardest.
I've seen people cough up nasty stuff after a session. They said it felt like their lungs finally saying 'thank you'.
Maybe could share this with older folks who hate pumping meds all day? Just a thought. Stay fresh, keep those lungs happy!
Steve Batancs
July 25, 2025 AT 09:53Chest percussion, though an ancient technique, remains supported by formal rehabilitation protocols internationally. Various guidelines emphasize its efficacy in secretion mobilization for patients with restrictive lung diseases and cystic fibrosis. That said, indiscriminate application without medical supervision risks complications — contusions, rib fractures among them.
The article rightly underscores the significance of adhering to validated therapeutic protocols issued by respiratory therapy authorities.
In sum, it’s imperative we recognize such hands-on methods as complementary and not replacements for primary pharmacological interventions.
elvin casimir
July 26, 2025 AT 06:43All I’m saying is people need to be careful. Chest percussion isn’t a magic trick or a free pass to skip proper treatment. If done wrong, you’re risking your ribs, your chest wall. It’s not a toy.
The grammar issues in the article don’t help either; it lessens the credibility when advice looks rushed or poorly edited. If you’re gonna write medical content, get your facts and your language straight.
Otherwise, sure, it might help but only under strict supervision.
Richa Ajrekar
July 27, 2025 AT 06:40@Virat I get that you like traditional methods but that doesn't mean everything old is gold. Proper medical advice matters because people's lives are at stake. And I’m not against natural remedies; I’m against misleading people.
Perhaps the article should have provided more scientific citations instead of just anecdotal recommendations. That would elevate the discussion beyond just good intentions.
Just hoping everyone stays safe and informed, not blindly hopeful.