Diabetic Peripheral Neuropathy is a chronic nerve disorder that primarily affects the feet and lower legs of people with diabetes, resulting from prolonged high blood sugar damaging peripheral nerves.
When blood glucose stays elevated for years, the tiny blood vessels that feed nerves get clogged. The nerves lose the ability to send and receive signals, leading to pain, tingling, or numbness. This condition is one of the most common diabetic peripheral neuropathy complications and can dramatically lower quality of life if caught late.
Why the nerves go rogue: Core causes
Three biological forces drive the nerve damage:
- Hyperglycemia - excess glucose creates harmful by‑products that attack nerve fibers.
- Oxidative stress - free radicals overwhelm the body’s antioxidant defenses, eroding nerve membranes.
- Microvascular disease - narrowed capillaries cut off oxygen and nutrients to the nerves.
These mechanisms don’t work in isolation. For example, a study from the American Diabetes Association found that each 1% rise in HbA1c increases the risk of peripheral neuropathy by roughly 30%.
Diabetes mellitus is a metabolic disease characterized by chronic hyperglycemia resulting from defects in insulin secretion, insulin action, or both. Managing blood sugar is the single most powerful lever to slow or even halt nerve damage.
Spotting the warning signs
The early stage often feels like a subtle “pins‑and‑needles” sensation. If you ignore it, the problem can progress to:
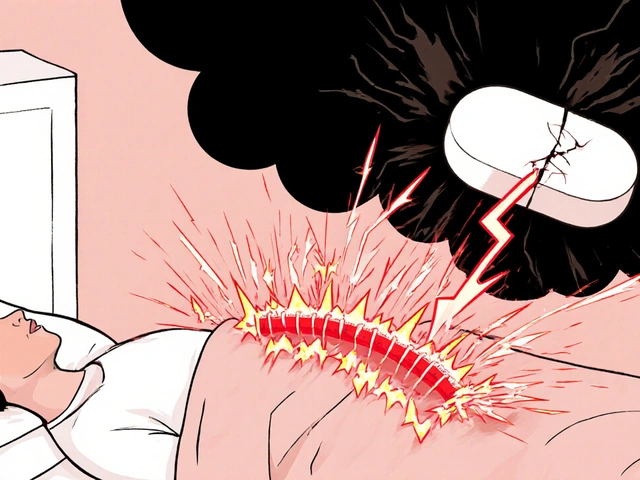
- Burning pain that worsens at night.
- Loss of temperature perception - you might not notice a hot pan.
- Muscle weakness leading to balance issues.
- Foot ulcers that heal slowly because the nerves can’t signal pain.
Because the nerves are compromised, patients frequently develop infections that can become life‑threatening. A simple foot inspection each morning can catch a tiny cut before it spirals.
How doctors diagnose the condition
Diagnosis blends patient history with objective tests:
- Physical exam - checking reflexes, vibration sense, and monofilament testing.
- Nerve conduction studies - measuring the speed of electrical signals along the nerve.
- Quantitative sensory testing - using devices to gauge temperature and pressure thresholds.
These tools help differentiate diabetic peripheral neuropathy from other causes like vitamin B12 deficiency or lumbar spine issues.
Treatment roadmap: From lifestyle to medication
Effective management rests on three pillars: tight glucose control, symptom relief, and nerve‑protective strategies.
1. Tight glucose control
Targeting an HbA1c below 7% (or the individualized goal set by your provider) can cut the progression risk by up to 50%. Tools that help include:
- Continuous glucose monitors (CGM) - provide real‑time trends.
- Structured carbohydrate counting - reduces post‑meal spikes.
- Regular physical activity - improves insulin sensitivity.
2. Pain‑modifying medications
When nerve pain becomes disruptive, doctors often turn to first‑line agents:
| Medication | Mechanism | Typical Dose | Common Side Effects |
|---|---|---|---|
| Duloxetine | Serotonin‑norepinephrine reuptake inhibitor | 30‑60mg daily | Nausea, dry mouth, fatigue |
| Pregabalin | Calcium channel α2‑δ ligand | 150‑300mg daily | Dizziness, edema, weight gain |
| Gabapentin | Calcium channel α2‑δ ligand | 900‑1800mg daily | Somnolence, ataxia, mood changes |
Switching between these agents or adding low‑dose tramadol is common if side effects limit adherence.
3. Nerve‑protective supplements
Alpha‑lipoic acid (600mg daily) and acetyl‑L‑carnitine have modest evidence for improving nerve conduction speed. Always discuss with your endocrinologist before starting any supplement.
4. Foot care and physical therapy
Custom orthotics, regular podiatrist visits, and gentle strengthening exercises preserve balance and prevent ulcer formation. One UK cohort showed a 40% drop in amputation rates when a multidisciplinary foot‑care team was involved.

Living with DPN: Everyday hacks
Practical adjustments can make a big difference:
- Wear breathable, well‑fitting shoes - avoid tight toe boxes.
- Use a daily foot mirror or enlist a partner to inspect soles.
- Apply a moisturizer at night but keep between toes dry to prevent fungal growth.
- Schedule glucose checks after meals and note any spikes that correlate with worsening tingling.
Mindfulness and stress‑reduction techniques also lower perceived pain, likely by modulating central pain pathways.
When to seek specialist care
If you notice any of the following, book an appointment promptly:
- Rapidly spreading numbness or weakness.
- Foot ulcer that doesn’t improve in a week.
- Uncontrolled blood sugar despite lifestyle changes.
- Severe, burning pain that disrupts sleep.
Neurologists, endocrinologists, and podiatrists often collaborate to tailor a plan that balances glucose targets with symptom control.
Related concepts and next steps
Understanding DPN opens the door to broader diabetes management topics. You might explore:
- Microvascular complications (retinopathy, nephropathy).
- Impact of weight loss surgery on nerve health.
- New therapeutic trials targeting nerve regeneration.
Each of these areas builds on the same foundation: controlling blood sugar and protecting small blood vessels.
Frequently Asked Questions
Can I reverse diabetic peripheral neuropathy?
Complete reversal is rare, but aggressive glucose control, lifestyle changes, and early treatment can halt progression and sometimes improve symptoms.
How often should I check my feet?
At least once daily. Use a mirror or have a partner help you look for cuts, calluses, or discoloration.
What HbA1c level reduces the risk of nerve damage?
Targeting an HbA1c under 7% (or the personalized goal set by your doctor) cuts the risk by roughly half compared to levels above 8%.
Are over‑the‑counter creams effective for neuropathic pain?
Topical lidocaine or capsaicin can provide modest relief for mild symptoms, but prescription agents remain the most evidence‑based options for moderate‑to‑severe pain.
Should I stop exercising if my feet are numb?
No. Low‑impact activities like swimming or cycling keep circulation flowing and improve glucose control, which actually protects nerves. Just avoid high‑impact sports that could cause injury.
What are the newest drugs in the pipeline for DPN?
Research is focusing on nerve‑growth factors such as NGF‑mimetic agents and oral formulations of baclofen‑enriched antioxidants. PhaseII trials show promise but are not yet commercially available.
Is dietary supplementation with B‑vitamins helpful?
Vitamin B12 deficiency can mimic neuropathy, so correcting low levels helps. However, routine high‑dose B‑vitamin supplementation hasn't shown consistent benefit unless a deficiency is documented.
How does smoking affect DPN?
Smoking worsens microvascular disease, accelerating nerve damage. Quitting can improve blood flow and may slow symptom progression.




barry conpoes
September 27, 2025 AT 18:55As an American, I find it astounding how many overseas guidelines ignore the superior standards of our healthcare system, especially when it comes to managing diabetic neuropathy. The research from top US institutions consistently outpaces European counterparts, proving that our approach to glucose monitoring and foot care is the gold standard. If you’re still following outdated protocols, you’re doing a disservice to yourself and your patients.
Kristen Holcomb
October 2, 2025 AT 10:02Thanks for sharing your perspective. While the US does have leading research, it's also crucial to consider diverse patient experiences. Incorporating community‑based foot‑care programs can bridge gaps that even top‑tier studies sometimes overlook, especially in underserved areas.
justin davis
October 7, 2025 AT 01:09Wow!!! You actually think that a simple CGM can replace years of lifestyle changes???! Let’s not forget that insulin therapy, diet, and exercise are still the backbone of any regimen-no magic device will save you from a bad diet!!!
Sukanya Borborah
October 11, 2025 AT 16:15Look, justin, your sarcasm is noted but the reality is that metabolic dysregulation isnt just a buzzword-it's a cascade of oxidative stress, microvascular compromise, and glycation end‑products that you cant just brush off with a meme.
bruce hain
October 16, 2025 AT 07:22While many laud US protocols, alternative evidence warrants cautious appraisal.
Dennis Owiti
October 20, 2025 AT 22:29I get where you're coming from, and it's true that over‑reliance on any single approach can blind us to holistic care. Balancing medication with daily foot checks and patient education often yields the best outcomes.
Justin Durden
October 25, 2025 AT 13:35Exactly, Dennis. Encouraging patients to set realistic glucose targets while celebrating small wins can keep them motivated without feeling overwhelmed.
Stu Davies
October 30, 2025 AT 03:42Great points everyone! 😊 It’s amazing how a community can share such practical tips and keep each other accountable.
Sally Murray
November 3, 2025 AT 18:49Indeed, Stu. From a sociocultural standpoint, the quotidian rituals of foot inspection embody a broader ethic of self‑care that transcends mere biomedical intervention.
Bridgett Hart
November 8, 2025 AT 09:55Diabetic peripheral neuropathy remains a formidable challenge in modern medicine. It is a condition that exemplifies the intersection of metabolic dysfunction and neurodegeneration. The pathophysiology is rooted in chronic hyperglycemia which initiates a cascade of molecular insults. Oxidative stress damages neuronal membranes and impairs axonal transport. Microvascular compromise further deprives nerves of essential nutrients. Consequently patients experience a spectrum of sensory disturbances. The clinical presentation often begins with paraesthesia that progresses to debilitating pain. Management must therefore be multifaceted. Tight glycemic control is non negotiable and should be pursued relentlessly. Pharmacologic agents such as duloxetine or pregabalin provide symptomatic relief but are not curative. Adjunctive therapies including alpha lipoic acid show modest benefit yet require physician oversight. Foot care protocols are indispensable to prevent ulceration and possible amputation. Multidisciplinary teams comprising endocrinologists podiatrists and physiotherapists enhance patient outcomes. Emerging research into nerve growth factors promises future therapeutic avenues. Ultimately a patient centered approach that integrates evidence based medicine with individualized care will mitigate the burden of this disease.
Sean Lee
November 13, 2025 AT 01:02From a systems biology perspective, the dysregulated insulin signaling cascade precipitates a maladaptive neuroinflammatory milieu that accelerates axonal degeneration.
Michael Christian
November 17, 2025 AT 16:09That's a solid take Sean and keeping things simple with regular walks and low‑impact cardio can really help maintain circulation without overtaxing the nerves.
Steven Elliott
November 22, 2025 AT 07:15Sure, because everyone loves being told to count carbs and wear orthotic shoes-what a revolutionary concept.
ankush kumar
November 26, 2025 AT 22:22ankush, i totally feel you man its like the healthcare system sometimes feels like a maze and we keep hearing the same advice over and over again about glucose monitoring and foot checks but what i think could really make a difference is community support groups where people can share their daily struggles and successes together maybe even a simple whatsapp group where we can post pictures of our feet daily and remind each other to check for cuts or sores i know it sounds a bit crazy but you never know until you try and sometimes a little nudge from a friend can stop a bad ulcer before it even starts
Cameron White
December 1, 2025 AT 13:29cameron: while mainstream guides push for pharma solutions, it's worth questioning who profits from the endless cycle of medication and devices that keep us hooked on the system.