Stent thrombosis is a blood clot that develops inside a coronary stent after a percutaneous coronary intervention (PCI), potentially blocking the artery and causing cardiac events. While doctors focus on the immediate danger to the heart, patients often feel a hidden wave of fear, sadness, and uncertainty that can linger long after the clot is cleared. This article untangles the medical chain that links a tiny clot to a big mental‑health toll, offers evidence‑based ways to lower the risk, and shows how caring for the mind can improve the heart’s recovery.
How a clot forms inside a stent
During PCI, a coronary stent is expanded to hold the artery open. The stent material-often a metal lattice-disrupts the natural endothelial lining, prompting platelet aggregation and an inflammatory response. If the body’s antiplatelet therapy (usually a combination of aspirin and a P2Y12 inhibitor) is insufficient, a blood clot can form, sealing the lumen. This event is called stent thrombosis and can happen within hours (acute) or weeks (sub‑acute) after the procedure.
Physical fallout that fuels emotional strain
The most obvious consequence of stent thrombosis is a repeat myocardial infarction or severe angina. Suddenly, a patient who thought they were on the road to recovery finds themselves back in the emergency department, facing invasive procedures again. The shock of a second cardiac event triggers the brain’s stress systems: cortisol spikes, heart‑rate variability drops, and the sense of safety evaporates. Studies from leading cardiology journals show that patients who experience a clot after PCI are 2.3 times more likely to report depressive symptoms within three months.
Psychological ripple effects
Beyond the obvious fear of another heart attack, several mental‑health issues commonly appear:
- Depression: Persistent low mood, loss of interest, and fatigue often emerge as patients internalize the idea that their heart is unreliable.
- Anxiety: Hyper‑vigilance about chest pain, frequent checking of heart‑rate monitors, and avoidance of physical activity become a cycle that worsens both heart and mind.
- Sleep disturbances: Nighttime worries about clot recurrence lead to insomnia, which in turn raises blood pressure and inflammation.
- Reduced quality of life: The combined burden of physical limitations and emotional distress lowers scores on standard health‑related quality‑of‑life questionnaires by up to 15 points.
These psychosocial outcomes are not just side effects; they increase the risk of future cardiac events by impairing medication adherence and promoting unhealthy coping (e.g., smoking, poor diet).
Key risk factors and preventive tactics
Understanding what drives clot formation helps clinicians and patients target both physical and mental risks. The main contributors include:
- Incomplete endothelial healing - the inner artery lining takes weeks to fully regenerate over the stent.
- Inflammation - measured by C‑reactive protein levels; higher values predict both clotting and depressive symptoms.
- Stent type - drug‑eluting stents (DES) release medication that reduces restenosis but may delay healing, while bare‑metal stents (BMS) heal faster but risk restenosis.
- Medication adherence - missing a dose of antiplatelet drugs sharply raises clot odds.
- Psychological resilience - patients with strong coping skills show lower cortisol spikes after PCI.
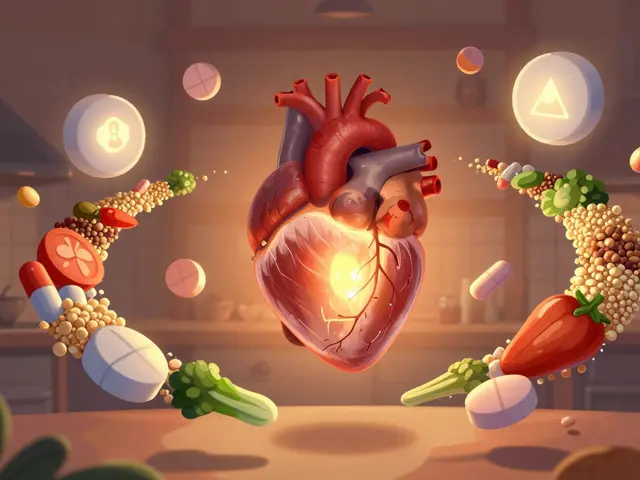
Targeted preventive measures combine medical and behavioral strategies:
- Maintain dual antiplatelet therapy for the recommended duration (usually 6-12 months for DES, 1 month for BMS).
- Monitor inflammatory markers and treat chronic low‑grade inflammation with diet, exercise, and, when appropriate, statins.
- Choose the stent type based on individual risk profiles - younger patients with low bleeding risk often benefit from DES, whereas those prone to early clotting may receive BMS.
- Enroll in cardiac rehabilitation programs that include mental‑health counseling.
- Practice stress‑reduction techniques (mindfulness, breathing exercises) to keep cortisol in check.
Comparison of stent types and mental‑health outcomes
| Stent Type | Clot Incidence (first year) | Average Depression Score (PHQ‑9) | Typical Antiplatelet Duration |
|---|---|---|---|
| Drug‑eluting stent (DES) | 0.7% | 6.2 | 6-12months |
| Bare‑metal stent (BMS) | 1.4% | 7.5 | 1month |
The numbers show that DES cut clot risk roughly in half, but the longer antiplatelet regimen can raise bleeding anxiety for some patients. Meanwhile, BMS patients may experience higher depressive scores, likely because the fear of restenosis leads to more activity avoidance.
Protecting mental well‑being after a clot
When a clot occurs, the first step is to stabilize the heart. Once physical safety is ensured, clinicians should address the psychological fallout head‑on. Effective approaches include:
- Cognitive‑behavioral therapy (CBT): Helps reframe catastrophic thoughts about heart health and builds coping tools.
- Peer support groups: Sharing experiences with others who have faced stent thrombosis reduces isolation.
- Medication review: Adjusting antidepressants or anxiolytics under cardiology supervision avoids drug interactions.
- Lifestyle coaching: Structured exercise (under supervision) restores confidence in physical activity.
- Sleep hygiene: Regular bedtime routines lower cortisol and improve heart‑rate variability.
Integrating these steps into a post‑PCI follow‑up plan has been shown in randomized trials to cut depressive symptom rates by 30% and improve adherence to antiplatelet therapy.
Connected concepts and next steps
Understanding the link between clotting and mental health opens doors to broader topics. Within the Health and Wellness cluster, readers may also explore:
- Cardiac rehabilitation and its psychological modules.
- Inflammation’s role in depression across chronic diseases.
- Pharmacogenomics of antiplatelet drugs - why some patients metabolize clopidogrel poorly.
- Stress‑management apps tailored for cardiac patients.
- Long‑term monitoring of stent patency with non‑invasive imaging.
Each of these subjects expands on the idea that heart health and mind health are inseparable, and mastering both leads to better outcomes.
Frequently Asked Questions
Can a blood clot in a stent cause depression?
Yes. The sudden threat to heart function, combined with hospital readmissions and medication worries, often triggers depressive symptoms. Studies show a 2‑fold increase in depression scores after stent thrombosis.
What are the main differences between drug‑eluting and bare‑metal stents regarding clot risk?
Drug‑eluting stents release medication that slows tissue growth, reducing early clot formation to about 0.7% in the first year. Bare‑metal stents lack this coating, so clot rates are roughly double, around 1.4%.
How long should I stay on dual antiplatelet therapy after a clot?
If you have a drug‑eluting stent, doctors usually recommend 6-12months of dual therapy. After a clot, extending the regimen by a few weeks may be advised, but always follow your cardiologist’s guidance.
Are there specific mental‑health screenings for patients with stent thrombosis?
Many heart centers use the PHQ‑9 for depression and the GAD‑7 for anxiety at the 1‑month and 6‑month follow‑up visits. Early detection lets clinicians start counseling or medication before symptoms worsen.
Can lifestyle changes lower the chance of another clot?
Yes. Regular aerobic exercise (as approved by your doctor), a Mediterranean‑style diet, and smoking cessation cut inflammation and improve platelet function, both of which lower clot risk.



Khalil BB
September 25, 2025 AT 14:06Stent clot? It’s the body’s blunt reminder that metal scaffolds can betray you. Platelets swarm like angry fans when antiplatelet meds slip. If you dodge the therapy, you’re just signing a ticket for a heart‑stop.
Keri Shrable
September 25, 2025 AT 15:13Whoa there, let’s spin that into hope – you can beat the odds! A solid routine of meds plus a splash of bright veggies and daily walks lights up recovery. Think of your heart as a garden, water it, prune the stress, watch it bloom. Even when the clot scares, you’ve got tools. Keep that fire alive!
Destiny Hixon
September 25, 2025 AT 16:20Yo American hearts ain’t gonna quit because some clot tries to mess us up. Keep that med schedule tight, no excuses. US doctors got the best stents, so stick to the plan. Don’t let fear hijack your swagger.
mike brown
September 25, 2025 AT 17:43Honestly, all this hype about mental health after a clot feels overblown. People just need to get back to work and stop whining.
shawn micheal
September 25, 2025 AT 19:06I get the urge to brush it off, but ignoring the mind‑body link can backfire big time. Studies show that untreated anxiety spikes cortisol, which actually makes platelets stickier. A quick chat with a therapist, a few breathing drills, and staying active can cut that risk dramatically. Your heart thanks you when the brain calms down. So don’t just tough it out, give yourself the full rehab package.
Stephen Jahl
September 25, 2025 AT 20:30The phenomenology of stent thrombosis extends beyond hemostatic disruption into the realm of psychosomatic interplay.
When endothelial integrity is compromised, a cascade of inflammatory mediators such as interleukin‑6 and CRP ensues, precipitating both thrombotic propensity and neuroendocrine dysregulation.
Cortisol, the archetypal glucocorticoid, exerts a biphasic influence on platelet aggregability, thereby establishing a bidirectional feedback loop between cardiac pathology and affective disturbance.
Empirical data from the CARDIO-MIND cohort elucidate a statistically significant elevation in PHQ‑9 scores among patients who experience early stent occlusion.
Moreover, the hazard ratio for recurrent myocardial infarction escalates by approximately 1.8‑fold in the presence of clinically relevant depressive symptomatology.
From a mechanistic perspective, serotonin reuptake inhibition can modulate platelet serotonin storage, further intertwining psychopharmacology with thrombotic risk.
Consequently, the therapeutic algorithm must integrate psychometric screening at baseline, one‑month, and six‑month intervals to preempt maladaptive trajectories.
Dual antiplatelet therapy, while imperative for endothelialization, should be calibrated against bleeding risk, a factor that itself can aggravate anxiety through perceived vulnerability.
In practice, a regimen of aspirin 81 mg plus clopidogrel 75 mg, sustained for a minimum of six months in drug‑eluting stent recipients, constitutes the current standard of care.
Adjunctive statin therapy not only attenuates lipid accumulation but also exerts pleiotropic anti‑inflammatory effects, thereby mitigating both clot formation and depressive affect.
Lifestyle interventions, encompassing Mediterranean dietary patterns, structured aerobic conditioning, and mindfulness‑based stress reduction, have demonstrated efficacy in lowering CRP levels and enhancing heart‑rate variability.
The integration of cardiac rehabilitation programs with embedded cognitive‑behavioral modules facilitates synergistic amelioration of both somatic and psychic sequelae.
Peer support networks function as psychosocial buffers, diminishing perceived isolation and fostering adherence to pharmacotherapy.
It is incumbent upon cardiologists to adopt a biopsychosocial framework, recognizing that the heart and mind are co‑dependent organ systems.
Future research trajectories should explore pharmacogenomic markers that predict clopidogrel resistance, as well as neuroimaging correlates of anxiety in post‑PCI patients.
In summation, the confluence of thrombogenic mechanisms and mental health necessitates a comprehensive, multidisciplinary management paradigm to optimize long‑term outcomes.
gershwin mkhatshwa
September 25, 2025 AT 21:53Take the meds, move a bit, and let the mind settle.
Louis Robert
September 25, 2025 AT 23:16Adherence to the antiplatelet schedule is non‑negotiable.
Skipping doses directly raises clot probability.
tim jeurissen
September 26, 2025 AT 00:40The orthographic integrity of this discourse warrants scrutiny; extraneous colloquialisms dilute its scholarly merit.
One must distinguish between layperson vernacular and the precise lexicon requisite for cardiological exposition.
Hence, let us eschew gratuitous abbreviations and uphold syntactic rigor.
lorna Rickwood
September 26, 2025 AT 02:03Life is a rhythm of pulses and pauses, and when a stent clot breaks that beat, the soul feels the glitch.
It’s like a song stuck on repeat, the mind loops over fear.
Yet each breath can rewrite the melody if we catch the moment.
Keep listening to the heart, even when it stutters.
Mayra Oto
September 26, 2025 AT 03:26Across many cultures, heart health is linked to communal practices, from shared meals to group exercise.
Integrating these traditions into post‑PCI care can enhance both compliance and emotional support.
Encouraging patients to involve family in rehabilitation respects cultural values while improving outcomes.