Picture this: back in the not-so-distant past, epilepsy treatment used to be all about flooding the brain with drugs that bluntly hammered sodium or GABA channels. And while those old-school medications did their job (sometimes too well), patients often paid the price with side effects—drowsiness, mood swings, cognitive dulling. Enter levetiracetam—a drug that took researchers by surprise. It calms seizures, but doesn’t touch sodium channels or even GABA directly. So how does it work? Here’s where things get interesting for any medical student who’s curious about what actually happens at the synapse.
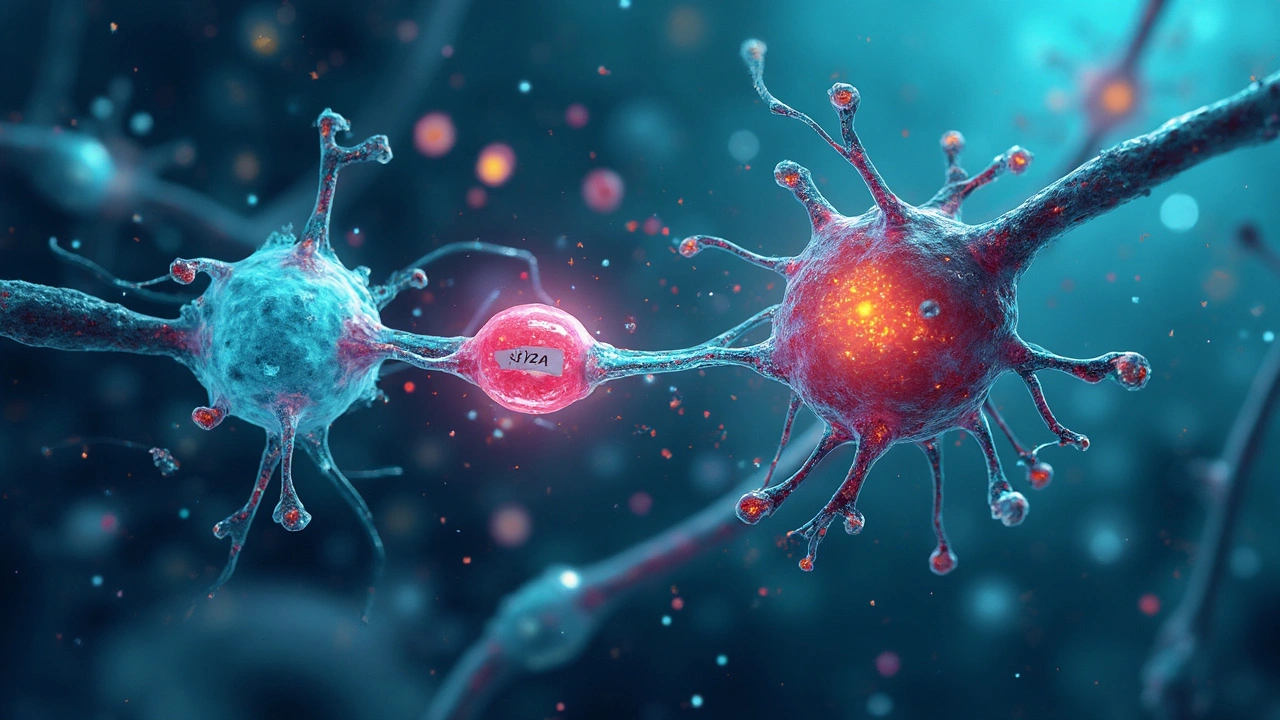
The Secret Target: Synaptic Vesicle Protein 2A (SV2A)
Leviteracetam’s claim to fame is its unique target—something overlooked for decades. Underneath the microscope, inside every presynaptic terminal, there’s a protein called synaptic vesicle protein 2A, or SV2A for short. This quirky little protein lives on the membrane of synaptic vesicles—the round, tiny sacks that store neurotransmitters ready to be fired off in a neural blitz. Now, not all vesicles, and not all proteins, are created equal. SV2A isn’t just wallpaper—it’s essential for vesicle function. It keeps vesicles primed and ready for release, almost like a pit crew keeps a race car in top shape before a critical F1 race. Without SV2A, the neuron’s ability to release neurotransmitters—especially during repetitive or high-frequency firing—runs into trouble.
Leviteracetam binds to SV2A with an impressive affinity. The binding happens right inside the brain—levetiracetam is designed to cross the blood-brain barrier seamlessly, so it gets right where the action is. This is the first truly selective SV2A ligand used clinically, and its specificity explains a lot about its tolerability compared to other anti-seizure meds. In 2008, the Nobel Prize-winning neuroscientist Dr. Roger Tsien pointed out,
“The focus on vesicle cycling proteins like SV2A is a whole different angle compared to the classic channel blockers. This shift opens up approaches to brain disorders that literally weren’t on the map before.”
Here’s something neat: studies show that when you knock out SV2A in mice, they have severe seizures—and binding capacity for levetiracetam vanishes. So, if someone ever asks if the action on SV2A is a side effect or the main deal, show them that knockout experiment. And as you’ll see in this levetiracetam mechanism of action deep-dive, this isn’t just coincidence—it’s the key to why the drug works.
How SV2A Binding Messes (Nicely) with Vesicle Dynamics
The minute levetiracetam grabs SV2A, it triggers a subtle, but powerful, change in how vesicles behave. Remember, SV2A isn’t opening or closing channels. Instead, it regulates how synaptic vesicles traffic, dock, and fuse at the presynaptic membrane. So what are the knock-on effects?
One practical way to look at it: levetiracetam tamps down on abnormally high vesicle release that occurs during the kind of electrical storms (paroxysmal depolarizations) you see in epilepsy. At baseline, the effect is mild—the drug doesn’t cramp normal firing patterns, which is why cognitive side effects are rare. But as soon as the neuron starts firing in weird, repetitive bursts (think temporal lobe epilepsy), levetiracetam blocks the vesicles’ overenthusiasm. A 2012 experiment found that synapses treated with levetiracetam showed a 40% reduction in stimulated neurotransmitter release, but no significant change in baseline transmission. That’s rare selectivity, and a lifesaver in practice.
So, what’s the consequence for the neuron? Less glutamate gets dumped into the synaptic cleft during seizures. But postsynaptic effects—like classic GABAergic drugs—don’t play a major role. Here’s a practical tip: if you’re on the wards and a consultant quizzes you on why levetiracetam doesn’t cause sedation like other antiepileptics, tell them it’s all about presynaptic modulation, not postsynaptic brain-muddling.
For reference, here’s a simplified breakdown to impress your study group:
| Step | What Happens |
|---|---|
| 1 | Levetiracetam crosses BBB and binds to SV2A on vesicles |
| 2 | SV2A-levetiracetam binding changes vesicle trafficking/fusion |
| 3 | Reduces excessive neurotransmitter (glutamate) release during seizures |
| 4 | Preserves normal neurotransmission and cognition |

Downstream Effects: What Really Happens after SV2A Modulation?
Once SV2A is modulated, downstream changes ripple through the synapse. The immediate outcome is fewer vesicles fusing with the presynaptic membrane under repetitive stress conditions. Think of it like turning down the volume knob—but only when the music is too loud. It’s not brute force inhibition, but a smart filtering process based on neuronal activity patterns.
For the postsynaptic neuron, the main result is less excitatory push, especially less glutamate. Glutamate is the chief “gas pedal” neurotransmitter of the brain, and when released in bursts, it throws neural circuits into chaos. By muting this surge, levetiracetam helps prevent the synchronized, wave-like firing that creates clinical seizures. In contrast, GABAergic drugs focus more on boosting inhibition, while sodium channel blockers blunt everything. This tailored modulation is why levetiracetam’s adverse reaction list is so much shorter—psychosis or agitation are rare but possible, usually in kids or those with prior psychiatric conditions.
Recent imaging studies using PET radioligands show SV2A occupancy at therapeutic doses is between 90–95%—demonstrating how tightly this interaction defines treatment success. Compare that to standard sodium channel blockers, where therapeutic and toxic doses often overlap. For medical students, remembering that levetiracetam hardly interacts with hepatic enzymes is key. It skips the CYP ballet—so fewer drug-drug interactions, great for polypharmacy cases in older patients or liver-compromised folks.
As for other downstream effects, animal research points to possible roles in stabilizing mitochondrial function and even tweaking synaptic plasticity—but these are still emerging ideas, not exam-room essentials yet. Clinical monitoring focuses on mood, behavior, and blood counts, but nothing like the hepatic watchlists for older antiepileptics. That’s one reason so many neurologists use levetiracetam as a first-line starter for new-onset epilepsy.
What Makes Levetiracetam Stand Out? Side Effects, Clinical Pearls, and Practical Tips
Medical students often ask—how is it possible that a single protein target means fewer side effects? Here’s why: levetiracetam’s high selectivity for SV2A means minimal off-target binding. Compare that to phenytoin or carbamazepine, which hit dozens of channels, and the picture becomes clear. The most common issues, like mild irritability, usually fade or respond to dose adjustments. Pediatric dosing is straightforward (no complex titration), and elderly patients tolerate it well.
Another clinical pearl: withdrawal is usually smooth, and you can begin or stop levetiracetam pretty rapidly in emergencies—there’s no risk of fatal rebound seizures like with benzodiazepines. Even status epilepticus protocols often include levetiracetam nowadays because of that flexibility. And don’t forget SV2A is now being investigated for roles in Alzheimer’s, depression, and even traumatic brain injury therapies—a testament to the protein’s broad neural importance.
If you’re trying to recall the most vital points for exams or wards:
- levetiracetam mechanism of action: presynaptic SV2A modulation
- Minimal effect on sodium, calcium, or GABA channels
- Low interaction with enzymes, few drug-drug issues
- Rarely causes significant sedation or weight gain
- Can help in a wide range of seizure types—focal, generalized, myoclonic
One tip—if you ever see a patient suddenly having mood swings on levetiracetam, check for sleep deprivation, recent stress, or preexisting psych history. Most can continue the drug with support, but alternatives are available if things escalate.

Putting It Together: Quick Guide and What’s Next in SV2A-Directed Therapies
The journey from bench science to bedside practice with levetiracetam shows what happens when researchers stop looking at the usual suspects (sodium and GABA receptors) and start digging into the “background crew” like SV2A. This approach doesn’t just stop at epilepsy. Newer drugs in the same SV2A ligand family (like brivaracetam) show even higher potency and may tweak the mechanism for other disorders. Think of SV2A as the conductor of vesicle symphony—if the conductor can adjust the timing just right, the music plays smoothly without the drama of missed notes and crashes.
In clinical practice, this means safer treatment, easier management for both docs and patients, and a clean track record for tolerability. If you’re sitting exams or prepping for clinical years, memorize SV2A, understand presynaptic modulation vs. direct inhibition, and remember the unique lack of hepatic enzyme involvement. And when you want a deeper dive or need to settle a debate, check out the classic review at this levetiracetam mechanism of action link—you’ll be the one in your cohort with the actual inside scoop.



byron thierry
July 17, 2025 AT 23:15What a brilliant breakdown! This explanation really nails how levetiracetam works on a molecular level without getting bogged down in the usual neurotransmitter jargon. 😎 It's fascinating how SV2A acts like a kind of traffic controller at the synapse—makes you appreciate the complexity beneath what might seem like a straightforward antiepileptic.
I'm curious—do you think this mechanism explains why levetiracetam tends to have fewer side effects compared to other antiepileptics? If it's more targeted, that might make sense. Definitely going to bookmark this for my studies.
bob zika
July 19, 2025 AT 04:10Indeed, the metaphor of the synaptic vesicle protein 2A as a key regulator is highly enlightening...!!! This layered perspective is invaluable for medical students aiming to grasp pharmacodynamics at a conceptual yet practical level. Furthermore, the inclusion of direct links for extended learning is commendable—such resources are paramount.
Has anyone noticed if this focus on SV2A has led to new drug development angles? The potential here seems vast!!!
Tommy Mains
July 19, 2025 AT 22:05Hey everyone, great thread here! Just to add some clarity: SV2A's role isn't just about calming seizures but modulating neurotransmitter release in a nuanced way that avoids major dopaminergic or serotonergic disruptions, which is why levetiracetam is often well-tolerated.
From a teaching perspective, I find that relating this to the idea of a 'dimmer switch' rather than an 'on/off' lever helps students grasp the subtlety of the mechanism. It’s not a full shutdown but a modulation that prevents over-excitation — the hallmark of seizures.
Anyone else tried this metaphor in their teaching?
Alex Feseto
July 22, 2025 AT 04:06While the content attempts to simplify levetiracetam’s mechanism of action, it inevitably glosses over the multifaceted and still somewhat obscure biochemical interactions governing SV2A binding. Concededly, for pedagogical purposes, such simplification may be warranted; nevertheless, I must urge caution against accepting these metaphors as comprehensive truths. Rigorous scholarship demands more nuanced scrutiny.
vedant menghare
July 23, 2025 AT 09:16This explainer really paints a vivid picture! The way SV2A is described almost brings a living character into the synapse, kind of like an unsung hero managing chaos quietly. It’s refreshing to see scientific mechanisms described with such warmth and creativity whilst remaining rigorous.
From the lens of cultural sharing in education, such storytelling may aid diverse learners who might struggle with dry texts. Could this method extend effectively to other complex pharmacodynamics topics?
Kevin Cahuana
July 25, 2025 AT 16:16Really appreciate the breakdown here, especially for its middle ground between technical depth and digestibility. It’s the kind of resource that helps bridge the gap between rote memorization and genuine understanding.
Seeing the function of SV2A framed through relatable metaphors truly assists in retention. As someone mentoring students, this approach encourages curiosity rather than dread around pharmacology.
Have others found such analogies impactful in their learning or teaching?
Danielle Ryan
July 27, 2025 AT 23:16Honestly, I can't help but wonder if all these explanations are just the surface glossing over what Big Pharma wants you to see. 🤔 This 'weird molecule' being a star? More like a pawn in their conspiracy to keep us hooked on meds that control our minds but don’t cure anything!!!
What if the whole mechanism is a smokescreen and the real effect is something else entirely? Can anyone confirm that we really understand what’s going on here, or are we just fed polished stories to calm us down?
Robyn Chowdhury
July 29, 2025 AT 02:46Hmm, I found the metaphors somewhat overplayed and the delivery a bit too eager to please. 😒 Sometimes less is more. The hype around levetiracetam feels a bit theatrical—like it’s trying too hard to be 'the answer' in epilepsy management. I mean, sure, it’s useful, but let’s not elevate it beyond its due.
Does everyone really need the whole 'star molecule' spiel? Maybe a straightforward factual presentation would suffice 🤷♀️.
Anyone else feel this way?
😏Deb Kovach
August 3, 2025 AT 21:40Really appreciate the educational effort! The use of relatable comparisons makes the complex mechanism far easier to grasp, especially for those still new to neuropharmacology. 😊
One thing I’m curious about — does the SV2A binding affect all types of neurons equally, or is there selectivity in different brain regions? That detail could be helpful to understand the clinical nuances.
Thanks for a thoughtful post overall!
Sarah Pearce
August 9, 2025 AT 16:33ok so like, i just started on levetiracetam and this post kinda helped but tbh it still feels kinda confusing lol. i get that the drug works on SV2A and that it’s different from usual meds but can someone break down what happens next? like, what does it actually stop or start in the brain? anyone?
Also, side note, does this mean it has less mood effects than other epilepsy meds? cuz that’s what i’m worried about.
Ajay Kumar
August 16, 2025 AT 01:20Hey! This explanation does wonders for unpacking levetiracetam’s unique approach. It really highlights how sometimes, the simplest way to modulate brain excitability isn’t about heavy suppression but fine-tuning—like adjusting the volume instead of muting.
Given epilepsy’s diversity, understanding these nuances is key for tailoring therapy that’s both effective and tolerable. I appreciate how the article gently balances technical detail with accessibility — crucial for students and clinicians alike!
Would love to see more content like this across the gamut of neuropharmacology.