People hear that memantine “blocks glutamate” and nod along, but what does that actually mean for a brain that’s struggling with memory and daily tasks? Here’s the short promise: the drug aims to calm toxic glutamate noise without muting the useful signals your brain still needs. It won’t reverse Alzheimer’s, and the effects are modest, but for the right person and dose, it can steady the day.
This guide gives you the plain-English version of how memantine works, why it helps some people more than others, how to use it safely, and what the best studies actually found. Expect straight talk, simple analogies, and a few key numbers you can hold onto.
TL;DR: What Memantine Does and Why It Matters
- Memantine is an uncompetitive NMDA receptor blocker. It slips into the NMDA “channel” only when it’s open and overactive, cutting toxic glutamate noise but sparing normal signaling.
- Best evidence is in moderate to severe Alzheimer’s disease. Gains are modest: a bit more clarity, steadier daily function, and less agitation in some people.
- Standard dosing (immediate release): start 5 mg once daily, increase by 5 mg each week to 20 mg/day (10 mg twice daily). Adjust for kidney problems.
- Common side effects: dizziness, headache, constipation, sleep changes. Watch for confusion or hallucinations during early titration.
- Think of it as turning down the “toxic feedback” rather than boosting memory. It helps most when glutamate overdrive is part of the picture.
Search intent decoded: you likely want a precise, readable explanation of the memantine mechanism of action, plus practical dosing, safety, and evidence-without the fluff.
How Memantine Works: The Brain-Friendly Version
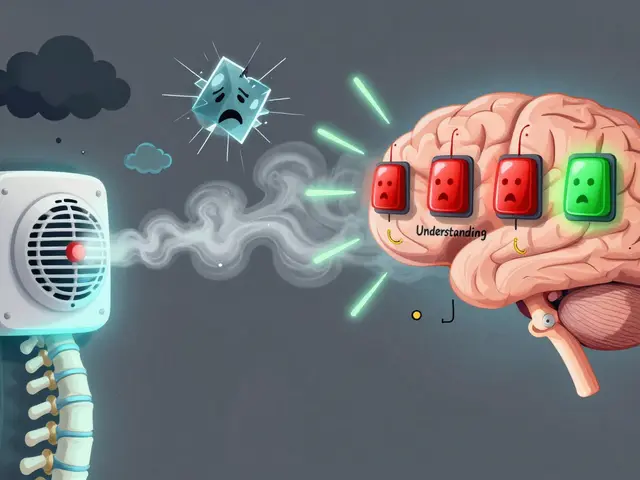
Glutamate is the brain’s main “go” signal. It talks to several receptors, but the NMDA receptor is the one tied to learning, plasticity, and-when it misfires-cell stress and death. In Alzheimer’s, amyloid and inflammation nudge glutamate signaling off balance. Synapses leak. Receptors stay active when they shouldn’t. That steady drip of over-activation is called excitotoxicity, and neurons hate it.
Here’s the trick: NMDA receptors are ion channels. They open when glutamate binds and voltage changes, letting calcium rush in. Too much calcium for too long triggers damage signals. A perfect drug would only block those receptors when they’re misbehaving, not when they’re doing honest work like encoding a face or a name.
Memantine gets close to that sweet spot. It’s an uncompetitive antagonist-translation: it only blocks the channel when it’s open and active. It binds inside the pore like a polite bouncer: “I’ll step in when things get rowdy and step out when the normal crowd arrives.” Two design features make this possible:
- Voltage dependence: The more the channel depolarizes (often during over-activity), the more memantine sticks. When the neuron is quiet, it lets go.
- Fast off-rate: When normal, brief pulses of glutamate arrive (the stuff you need for learning), memantine unplugs quickly. Fast on, fast off-so synaptic, time-limited signals can pass.
There’s another nuance: extrasynaptic vs synaptic NMDA receptors. Synaptic NMDA signaling is tied to healthy plasticity. Extrasynaptic signaling, when constantly dripped on by glutamate, flips on stress pathways. Lab work suggests memantine blunts extrasynaptic “harm” more than synaptic “help,” which matches its clinical profile: symptom steadiness without sedation (Lipton and colleagues; Hardingham & Bading; Parsons et al.).
What about other receptors? At therapeutic levels, memantine is pretty clean. It tickles a few others (like 5-HT3) at higher concentrations but not enough to explain its benefits. The main show is NMDA channel blocking with kinetics tuned to real-world brain firing.
Quick mental model: imagine a volume knob on toxic glutamate noise. Memantine turns it down during the loud parts but doesn’t mute the music.
| Property | Typical value | Why it matters |
|---|---|---|
| Half-life | ~60-80 hours | Slow washout; once or twice daily dosing is fine; changes show over weeks. |
| Oral bioavailability | ~100% | Food doesn’t matter much; dosing is simple. |
| Protein binding | ~45% | Low risk of protein-binding interactions. |
| Elimination | Renal (active tubular secretion; pH-dependent) | Urine alkalinization can raise levels; dose adjust in renal impairment. |
| Receptor action | Uncompetitive, voltage-dependent NMDA channel block | Blocks over-activation; spares normal synaptic signaling. |
Primary sources: EMA Summary of Product Characteristics; FDA Prescribing Information; BNF/NICE monographs; mechanistic work by Parsons CG et al., Lipton SA et al., and Hardingham GE & Bading (peer-reviewed).

Using Memantine in Real Life: Dosing, Safety, and Who Benefits
Who is most likely to benefit? People with moderate to severe Alzheimer’s disease-those needing help with daily tasks, showing agitation, or fluctuating confusion. Results are usually modest but meaningful for some families: steadier mornings, fewer outbursts, slightly better attention during conversations.
Who is unlikely to benefit? Mild Alzheimer’s or cognitive complaints without clear functional loss. Trials in mild disease show little to no advantage over placebo.
How long before you know? Give it 8-12 weeks at a stable target dose. Benefits, if they come, show as smoother days and slightly improved function rather than dramatic memory gains.
Dose and titration (immediate release, common UK/NHS practice):
- Week 1: 5 mg once daily
- Week 2: 10 mg/day (5 mg twice daily)
- Week 3: 15 mg/day (5 mg morning, 10 mg evening)
- Week 4: 20 mg/day (10 mg twice daily; usual maintenance)
Extended-release formulations exist in some regions. Follow local labeling if using a once-daily modified-release product. What matters most: slow, steady titration and watching the person, not just the dose.
Renal impairment (rule of thumb, check local guidance):
- Creatinine clearance 30-49 mL/min: consider max 10 mg/day for a week, then increase to 20 mg/day if tolerated.
- Creatinine clearance 5-29 mL/min: typical max 10 mg/day.
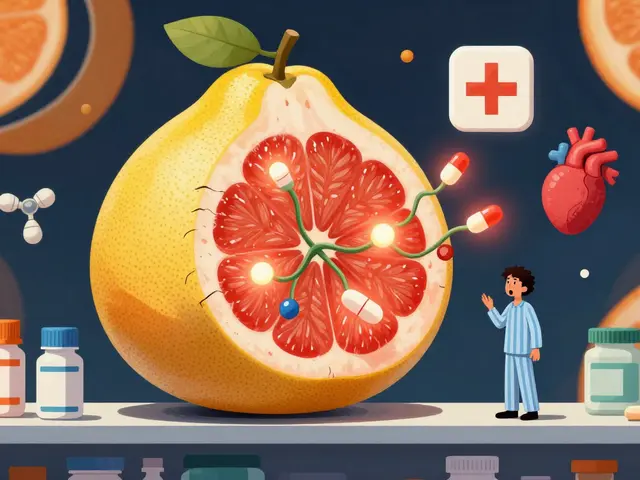
Memantine is cleared by the kidney and its clearance drops when urine is more alkaline. That’s why certain conditions and drugs can raise levels unexpectedly.
Interactions to keep on your radar:
- Urine alkalinizers: sodium bicarbonate, acetazolamide, or chronic vomiting can increase pH and memantine exposure. Watch for dizziness or confusion.
- Other NMDA blockers: amantadine, ketamine, dextromethorphan-risk of agitation, hallucinations, or odd behavior. Avoid combos if possible.
- Drugs using renal cation transport: the label mentions agents like cimetidine or quinidine; clinical impact is usually small, but be alert if the patient seems oversedated or spacey after a new med starts.
- Alcohol: can worsen confusion and balance issues; keep it minimal.
Common adverse effects: dizziness, headache, constipation, high blood pressure, somnolence or insomnia, and occasional confusion. Less common: hallucinations, aggressive behavior, or fainting-usually early on or during dose changes. People with a seizure history can usually take memantine, but uncontrolled epilepsy is a caution.
Compare with cholinesterase inhibitors (donepezil, rivastigmine, galantamine):
- Mechanism: cholinesterase inhibitors boost acetylcholine; memantine reduces glutamate overdrive. Different levers.
- Stage: cholinesterase inhibitors are often started in mild to moderate disease; memantine is most helpful in moderate to severe disease.
- Combo use: trials show small additive benefits when memantine is added to stable donepezil in moderate to severe stages.
What the evidence says (the gist):
- Reisberg et al., N Engl J Med 2003: in moderate to severe Alzheimer’s, memantine improved global status and activities of daily living vs placebo.
- Tariot et al., JAMA 2004: add-on to donepezil showed small but meaningful gains in cognition and function compared with donepezil alone.
- Howard et al., NEJM DOMINO-AD 2012: memantine gave modest improvements in cognition and daily activities when added or substituted in community-dwelling patients with moderate to severe disease.
- Meta-analyses: consistent but small effect sizes on cognition, global rating, and function in moderate to severe stages; minimal benefit in mild disease.
| Trial snapshot | Population | Main outcome | Takeaway |
|---|---|---|---|
| Reisberg 2003 | Moderate-severe AD | Better global/ADL scores vs placebo | Symptom-level gain; not a cure |
| Tariot 2004 | Memantine + donepezil | Improved cognition/function vs donepezil alone | Additive benefit in later stages |
| DOMINO-AD 2012 | Community-dwelling, mod-severe AD | Small gains in SMMSE, BADLS | Useful in routine care settings |
Citations: FDA Prescribing Information (Namenda); EMA SmPC; BNF/NICE; N Engl J Med and JAMA trials listed above. These are primary or guideline-level sources clinicians rely on.
Cheat Sheets, Examples, and Quick Answers You’ll Actually Use
Heuristic: Is memantine a good fit right now?
- Stage check: moderate to severe Alzheimer’s? Yes → consider. Mild disease? Unlikely to help.
- Goals check: aiming for steadier routine and fewer distressing behaviors? More likely to notice benefit.
- Risk check: renal impairment or urine alkalinization? Adjust dose and monitor.
- Combo check: already on donepezil and tolerating? Small additive benefit is possible.
One-month example (caregiver view): Week 1 on 5 mg: a bit of sleepiness by mid-afternoon. Week 2 at 10 mg: walking steadier, fewer angry outbursts in the evening. Week 3 at 15 mg: constipation pops up-add fluids and gentle laxative as needed. Week 4 at 20 mg: family notices he follows a TV show without pacing. Not dramatic, but the home feels calmer. If nothing changes by week 10-12, discuss scaling back.
Red flags during titration:
- Sudden confusion, agitation, or hallucinations: pause dose increases; consider stepping back one level.
- New falls or fainting: check blood pressure sitting and standing; review other meds.
- Persistent insomnia or vivid dreams: shift doses earlier in the day.
- Constipation not responding to basics: introduce a softener or osmotic laxative.
Checklist: Safe start in primary care
- Confirm stage (moderate to severe) and goals (comfort, function, behavior).
- Check eGFR; plan dose if eGFR < 30 mL/min/1.73 m².
- Scan meds for NMDA-active drugs (amantadine, ketamine, dextromethorphan).
- Ask about antacids/bicarbonate use, severe vomiting, or special diets that could alkalinize urine.
- Explain expected effects (modest, gradual) and side effects (dizziness, constipation).
- Set a review at 8-12 weeks to judge benefit.
Cheat sheet: Do vs Don’t
- Do titrate weekly and watch the person, not just the pill count.
- Do keep hydration and movement up to prevent constipation.
- Do treat sleep issues by shifting dose timing before adding sedatives.
- Don’t combine with ketamine, amantadine, or heavy cough syrup dosing.
- Don’t expect memory miracles; look for calmer routines.
Mini-FAQ
- Does memantine slow Alzheimer’s? It’s symptomatic. It may steady function for a time, but it isn’t a disease-modifying therapy.
- When will we see something? If it helps, most notice changes within 2-3 months at the target dose.
- Can we stop suddenly? You can, but a short taper (drop by 5-10 mg per week) helps you see if problems return and avoids misreading withdrawal as “worsening.”
- Is it addictive? No.
- What about vascular or Lewy body dementia? Evidence is mixed or limited. Use is off-label in many places; discuss with a specialist.
- Can memantine worsen agitation? Rarely, yes-especially early on or with interacting drugs. Back off the dose or stop if needed.
- What lab tests do we need? Mainly kidney function before and during long-term use, especially if health status changes.
For students: clean mechanism recap
- Target: NMDA receptor ion channel
- Antagonism: uncompetitive, voltage-dependent, fast off-rate
- Effect: reduces pathologic Ca²⁺ influx during tonic activation; spares phasic synaptic LTP
- Clinical tie-in: improves global status and ADLs modestly in moderate-severe AD
For clinicians: quick decisions
- Start 5 mg OD; up weekly to 20 mg/day (10 mg BD). Renal adjust as above.
- Define success with family: calmer evenings, less pacing, better wash/dress routines.
- Reassess at 8-12 weeks; stop if no clear benefit.
- Beware urine pH shifts raising exposure; review bicarbonate/antacid use.
For caregivers: practical moves
- Pair the pill with a daily habit (first tea of the day) to avoid missed doses.
- Keep a very short diary: sleep, mood, meals, odd events. It helps spot patterns.
- If mornings are groggy, move the larger dose to earlier evening.
- Ask about a bowel plan early if constipation shows up.
Disclaimer: This is general education, not personal medical advice. Always follow local guidance (BNF/NICE in the UK) and the prescriber who knows the person’s full story.

Next Steps and Troubleshooting Paths
If you’re a GP or prescriber:
- Confirm diagnosis and stage. If it’s mild, prioritise cholinesterase inhibitors and non-drug support.
- Start low, go slow. Book a 6-8 week check-in with caregiver-reported outcomes (sleep, agitation, ADLs).
- Hit a wall at 15-20 mg/day with side effects? Step back one titration level and hold for 2-3 weeks. Reassess.
- No benefit at 12 weeks? Agree on a taper and stop. Document the functional goals and why it didn’t help.
If you’re a caregiver:
- Watch patterns, not just single days. Two calmer weeks beat one rough afternoon.
- Bring notes to reviews: any falls, new meds, tummy issues, or sleep changes.
- Ask about constipation prevention on day one. It’s easier to prevent than chase.
- If behavior worsens right after a dose increase, call the prescriber and consider dropping back to the last well-tolerated dose.
If you’re a student or trainee:
- Be able to explain “uncompetitive, voltage-dependent block with fast off-rate” in a sentence-and why that spares normal LTP.
- Know the big trials and what they measured: global change scales, ADLs, and cognitive tests-not just MMSE.
- Remember the renal and urine pH angle. It’s exam gold and clinically real.
Troubleshooting decision cues:
- Early agitation after an increase? Reduce to prior dose; review for dextromethorphan or amantadine exposure.
- Sudden confusion with new antacid routine? Check if it includes bicarbonate; consider dose adjustment.
- No constipation plan and day 10 looks rough? Start an osmotic laxative, bump fibre and fluids, add gentle walks.
- Plateau at 10 mg/day with partial benefit and eGFR ≥ 50? Try 15 mg/day for two weeks, then 20 mg/day if still well tolerated.
Bottom line you can use tomorrow: memantine takes the edge off toxic glutamate activity without silencing useful signals. It’s most helpful in moderate to severe Alzheimer’s, with careful dosing and clear goals. Set expectations early, watch the person closely, and let the real-world outcomes guide your next move.



Erica Ardali
August 29, 2025 AT 23:50In the grand theater of neuropharmacology, memantine assumes the role of a subtle dramaturge, slipping onto the stage only when the NMDA receptors are over‑excited and demanding applause. It does not seek to rewrite the script of cognition but merely to mute the cacophony of toxic glutamate, allowing the remaining actors-learning, memory, and perception-to be heard. The elegance of an uncompetitive, voltage‑dependent block lies in its refusal to silence the essential dialogue of synaptic transmission, preserving the delicate balance required for plasticity. One might liken it to a seasoned conductor, lowering the volume of a blaring instrument without silencing the orchestra entirely. Thus, while it lacks the grandeur of a cure, its nuanced intervention offers a modest yet meaningful harmony for those navigating the frailties of Alzheimer’s disease.
Justyne Walsh
August 31, 2025 AT 03:37Oh, wonderful-another pharmaceutical hero to remind us that pushing chemicals into the brain is a moral triumph. Because what we really needed was a drug that claims to "tune down" glutamate while pretending it isn’t playing god. Sarcasm aside, the claims are as inflated as the rhetoric.
Callum Smyth
September 1, 2025 AT 07:24Sounds like you’ve got a solid roadmap for getting the most out of memantine 😊. Remember, titration is the key: the slow climb from 5 mg to 20 mg lets the brain adjust without being shocked. Keep an eye on side‑effects like dizziness or constipation, and involve the caregiver in tracking any changes. If the target dose arrives without noticeable benefit after 8‑12 weeks, it might be time to reassess the overall strategy.
Xing yu Tao
September 2, 2025 AT 11:10The mechanistic nuance of an uncompetitive NMDA antagonist such as memantine lies in its preferential occupancy of the channel pore during pathological over‑activation. By virtue of a voltage‑dependent binding affinity and a rapid dissociation kinetics, it spares physiologic synaptic events that underlie long‑term potentiation. This pharmacodynamic profile correlates with clinical observations of modest functional stabilization without overt sedation. Moreover, its renal clearance mandates dosage adjustments in compromised patients, underscoring the importance of individualized regimens. In sum, the drug offers a targeted attenuation of excitotoxicity while preserving essential neurotransmission.
Adam Stewart
September 3, 2025 AT 14:57From a practical standpoint, aligning dosing with renal function is paramount; a reduced eGFR means a lower maximum daily dose to avoid accumulation. Initiate at 5 mg daily and increment weekly, monitoring for dizziness, headache, or gastrointestinal upset. Encourage caregivers to record daily observations-sleep quality, mood swings, and any falls-to objectively gauge benefit. Should adverse events emerge, consider holding at the current tolerated dose before further titration. This methodical approach maximizes safety while giving the medication a fair trial.
Selena Justin
September 4, 2025 AT 18:44I appreciate the thoroughness of the guide and the balanced tone it maintains throughout. The emphasis on realistic expectations-modest gains rather than miracle cures-is both honest and compassionate. It is also helpful to see clear instructions on renal dose adjustments, which are often overlooked. Finally, the caregiver‑focused tips, such as maintaining a simple symptom diary, empower families to participate actively in the treatment process.
Bernard Lingcod
September 5, 2025 AT 22:30I wonder how the fast off‑rate of memantine compares in real‑world settings to the slower kinetics of other NMDA antagonists. Could this property be the reason we observe fewer cognitive blunts while still achieving neuroprotection? It would be valuable to see head‑to‑head studies that parse out these subtle pharmacodynamic distinctions.
Raghav Suri
September 7, 2025 AT 02:17Clinically, the distinction between synaptic and extrasynaptic NMDA blockade is paramount-memantine’s preferential dampening of the latter aligns with reduced excitotoxic cascades. In practice, this translates to modest improvements in daily functioning without suppressing learning capacity. Nevertheless, vigilant monitoring for early agitation or hallucinations remains essential during titration.
Freddy Torres
September 8, 2025 AT 06:04Memantine is the quiet bouncer that lets the brain’s party flow.
Andrew McKinnon
September 9, 2025 AT 09:50In the lexicon of neuro‑modulators, memantine is essentially a voltage‑gated, low‑affinity, once‑daily antagonist-nothing to write home about.
Dean Gill
September 10, 2025 AT 13:37Reading through the comprehensive overview of memantine’s mechanism, I was struck by how many layers of nuance are packed into what many consider a “simple” drug. First, the concept of an uncompetitive antagonist is itself a sophisticated pharmacological strategy, allowing the molecule to intervene only when the NMDA channel is actively open. This means that normal synaptic transmission, the cornerstone of learning and memory, remains largely untouched-a crucial point for clinicians concerned about blunting cognition further. Second, the voltage‑dependence adds another safeguard, ensuring that the drug’s binding affinity increases only when neuronal membranes are depolarized, which typically occurs during pathological over‑excitation. The fast off‑rate is a third elegant feature; it grants the drug the ability to quickly disengage during normal brief glutamate pulses, preserving the rapid signaling required for processes like long‑term potentiation. Moreover, the distinction between synaptic and extrasynaptic receptors provides a mechanistic rationale for the observed clinical profile: attenuation of excitotoxic stress without significant sedation. In terms of pharmacokinetics, the long half‑life of roughly 60‑80 hours offers convenient once‑or‑twice‑daily dosing, but also necessitates careful dose titration to avoid accumulation, especially in patients with renal impairment. The renal excretion pathway underscores the importance of adjusting doses based on eGFR, a detail sometimes missed in routine prescribing. From a safety standpoint, side effects such as dizziness, headache, and constipation are relatively mild, yet clinicians must remain alert for rare but serious events like hallucinations or severe agitation, particularly during the early titration phase. The evidence base, highlighted by pivotal trials such as Reisberg 2003 and the DOMINO‑AD study, consistently shows modest but meaningful improvements in global function and activities of daily living for patients with moderate to severe Alzheimer’s disease. While the effect sizes are small, they translate into real‑world benefits, such as steadier mornings and fewer behavioral outbursts, which can significantly ease caregiver burden. Finally, the practical guidance on integrating memantine with cholinesterase inhibitors expands therapeutic options, suggesting that a combined approach may yield additive benefits for certain patients. All told, the drug’s pharmacodynamic elegance, coupled with its clinical modesty, makes it a valuable tool in the therapeutic armamentarium for Alzheimer’s disease, provided it is used with careful patient selection, dosing, and monitoring.
Royberto Spencer
September 11, 2025 AT 17:24One could argue that the very act of dampening excitotoxicity reflects a deeper ethical commitment to preserving neuronal dignity, even if the gains are modest. Yet, the temptation to overstate its impact risks clouding the moral clarity we owe patients and families. The science demands humility, not hubris.
Annette van Dijk-Leek
September 12, 2025 AT 21:10What a brilliant breakdown!!! I love how every point is crystal clear!!! Keep sharing such gems!!!