Metoclopramide-Antipsychotic Interaction Checker
Check Your Medication Safety
This tool checks if your medications could cause a dangerous interaction that may lead to Neuroleptic Malignant Syndrome (NMS).
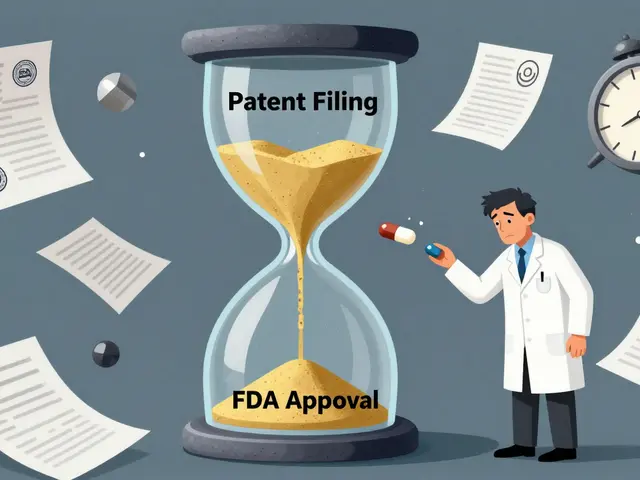
Combining metoclopramide with antipsychotic medications isn’t just a mild drug interaction-it’s a potentially deadly mix. If you or someone you know is taking both, you need to understand what’s really going on inside the body. This isn’t theoretical. People have died from it. The FDA has issued a clear warning: avoid metoclopramide in patients on antipsychotics. Yet, this combination still happens-often because doctors don’t realize how dangerous it is, or because patients aren’t told the full risk.
What Metoclopramide Actually Does
Metoclopramide, sold under brands like Reglan and Gimoti, is a drug meant to treat nausea, vomiting, and slow stomach emptying (gastroparesis). It works by blocking dopamine receptors in the brain and gut. That’s why it helps with nausea-it stops the signal in the brain’s vomiting center. But dopamine isn’t just about nausea. It’s a key chemical for movement, mood, and muscle control. The problem? Metoclopramide doesn’t just block dopamine in the stomach. It crosses into the brain and blocks dopamine receptors there too. That’s why it can cause tremors, muscle stiffness, and involuntary movements. The FDA added a Boxed Warning in 2017: long-term use can cause tardive dyskinesia, a permanent movement disorder. That warning alone should make any doctor pause. But when you add another dopamine blocker-like an antipsychotic-the risk skyrockets.How Antipsychotics Work (and Why That’s a Problem)
Antipsychotics like haloperidol, risperidone, and olanzapine were developed to treat schizophrenia and bipolar disorder. They work by blocking dopamine receptors in the brain’s reward and thinking pathways. That’s how they reduce hallucinations and delusions. But dopamine isn’t just about psychosis. It’s also essential for smooth, controlled movement. That’s why many people on antipsychotics develop side effects like muscle rigidity, shuffling walk, or tremors-exactly like Parkinson’s disease. These are called extrapyramidal symptoms (EPS). They’re common enough that doctors often prescribe extra meds to counter them. But when you add metoclopramide into the mix, you’re doubling down on dopamine blockade. Two drugs, same target, same effect-only now the brain is being hit twice as hard.Neuroleptic Malignant Syndrome: The Deadly Result
When dopamine blockade goes too far, too fast, the body can go into a state called Neuroleptic Malignant Syndrome (NMS). It’s rare-but when it happens, up to 20% of cases are fatal. NMS isn’t just “bad side effects.” It’s a full-body crisis. The classic signs are the “tetrad”:- High fever (over 102°F / 39°C)
- Severe muscle rigidity (so stiff you can’t move)
- Confusion, agitation, or loss of consciousness
- Unstable blood pressure, fast heart rate, sweating (autonomic instability)
Why This Interaction Is Worse Than You Think
It’s not just that both drugs block dopamine. There’s a second layer of danger: pharmacokinetics. Metoclopramide is broken down in the liver by an enzyme called CYP2D6. Many antipsychotics-like risperidone, haloperidol, and fluoxetine (an antidepressant often used with antipsychotics)-block that same enzyme. So instead of being cleared from the body, metoclopramide builds up. Your blood levels can double or triple. You’re not just getting two dopamine blockers-you’re getting a much stronger dose of one. This is especially risky for older adults, people with kidney disease, or those with genetic variations that make CYP2D6 work slowly. These people are already more sensitive to metoclopramide. Add an antipsychotic, and the risk isn’t just higher-it’s exponential.What Alternatives Are Safe?
If you’re on an antipsychotic and need help with nausea or gastroparesis, metoclopramide is not the answer. Here’s what doctors should be prescribing instead:- Ondansetron (Zofran): Blocks serotonin, not dopamine. Safe with antipsychotics.
- Methylprednisolone: Sometimes used for nausea in cancer patients.
- Promethazine: Works on histamine receptors. Use with caution due to sedation, but no dopamine blockade.
- Prochlorperazine: Also a dopamine blocker-so avoid it too.
Who’s at the Highest Risk?
This isn’t a risk that affects everyone equally. Certain groups are far more vulnerable:- People with Parkinson’s disease or a history of movement disorders
- Older adults (over 65)
- Patients with kidney problems (metoclopramide is cleared by the kidneys)
- Those taking multiple CNS drugs (antidepressants, antipsychotics, sedatives)
- People with a history of depression (metoclopramide can worsen it)
- Anyone who’s had tardive dyskinesia before
What to Do If You’re Already Taking Both
If you’re currently on metoclopramide and an antipsychotic, don’t stop either abruptly. Sudden withdrawal can cause rebound nausea or worsen psychiatric symptoms. But you need to act. Step 1: Get a full list of every medication you take-including over-the-counter pills, supplements, and herbal remedies. Step 2: Bring that list to your doctor or pharmacist. Say: “I’m on metoclopramide and [name of antipsychotic]. I’ve heard this can be dangerous. Can we review this?” Step 3: Ask for an alternative antiemetic. Ondansetron is usually the best choice. Step 4: Watch for early warning signs: muscle stiffness, fever, confusion, trouble moving. If you notice any of these, go to the ER immediately. NMS doesn’t wait.Why This Keeps Happening
You’d think this would be a no-brainer. But here’s why the interaction still occurs:- Doctors forget metoclopramide is a dopamine blocker-it’s often seen as just a “stomach medicine.”
- Patients don’t tell their psychiatrist they’re taking Reglan for nausea.
- Pharmacists don’t always catch the interaction if the drugs are prescribed by different doctors.
- Metoclopramide is cheap and widely available. It’s easy to reach for.
The Bottom Line
Metoclopramide and antipsychotics don’t just interact-they collide. The result can be fatal. There is no safe dose combination. No “low risk” window. No monitoring protocol that makes this okay. If you’re on an antipsychotic, metoclopramide should be off the table. Period. Use ondansetron instead. If you’ve been on metoclopramide for more than 12 weeks, you’re already at risk for permanent movement damage. If you’ve had any kind of muscle stiffness, tremors, or unusual movements since starting it, stop it now-and get help. This isn’t about being scared of medication. It’s about knowing what’s truly dangerous. And this interaction? It’s one of the most serious ones in modern medicine.Can metoclopramide cause Neuroleptic Malignant Syndrome on its own?
Yes, though it’s rare. Metoclopramide alone has been linked to cases of NMS, especially at high doses or in people with kidney problems. But the risk is much higher when combined with antipsychotics or other dopamine-blocking drugs. The FDA warns against using it with any drug associated with NMS, including antipsychotics, because the combination multiplies the danger.
How long does it take for NMS to develop after taking metoclopramide with an antipsychotic?
NMS can develop within hours or days. Most cases appear within the first week of starting or increasing the dose of either drug. Some reports show symptoms appearing as quickly as 24-48 hours after combining the two. There’s no safe waiting period-any new muscle stiffness, fever, or confusion after starting this combo should be treated as an emergency.
Is metoclopramide safe if I’m on an atypical antipsychotic like olanzapine or quetiapine?
No. The FDA’s warning includes both typical and atypical antipsychotics. Atypical antipsychotics like olanzapine, risperidone, and quetiapine still block dopamine receptors, even if they target other brain chemicals too. The combination still increases dopamine blockade enough to trigger NMS. There’s no “safer” antipsychotic in this context-avoid metoclopramide entirely.
What should I do if I’ve already taken metoclopramide with an antipsychotic and feel fine?
Even if you feel fine, you’re still at risk. NMS doesn’t always show symptoms right away. Stop taking metoclopramide immediately and talk to your doctor about switching to a safer alternative like ondansetron. Inform your pharmacist and psychiatrist so they can update your records. Monitoring for symptoms for at least two weeks is recommended, especially if you’ve been on the combo for more than a few days.
Are there any blood tests that can predict if I’m at risk for NMS?
There’s no test that predicts NMS before it happens. But once symptoms appear, doctors check creatine kinase (CK) levels, which rise when muscles break down. Other tests include electrolytes, liver enzymes, and kidney function. Genetic testing for CYP2D6 metabolism can show if you’re a slow metabolizer-which increases your risk-but this isn’t routinely done. The best prevention is avoiding the drug combo altogether.



Martin Viau
December 30, 2025 AT 20:46Let’s be real-this isn’t some obscure drug interaction, it’s a fucking death sentence waiting to happen. Metoclopramide? A dopamine sledgehammer. Antipsychotics? Another one. Combine ‘em and you’re basically running a neurological Chernobyl in someone’s basal ganglia. I’ve seen ER docs miss this because they think ‘Reglan’ is just for nausea. It’s not. It’s a neurotoxin with a prescription label. The FDA warning is there for a reason-stop pretending it’s a suggestion.
Marilyn Ferrera
December 31, 2025 AT 10:34Metoclopramide isn’t ‘just a stomach pill.’ It’s a CNS-active dopamine antagonist-period. And antipsychotics? Same mechanism. Double blockade = NMS risk. No gray area. No ‘maybe.’ This is pharmacology 101. If your doctor prescribes this combo, ask them to cite the safety data. They won’t. Because it doesn’t exist.
Robb Rice
December 31, 2025 AT 17:02I appreciate the thorough breakdown of the pharmacokinetics here. The CYP2D6 inhibition angle is especially critical-many clinicians overlook metabolic interactions when focusing solely on pharmacodynamics. It’s not just additive; it’s synergistic in the most dangerous way possible. Patients on multiple CNS agents, especially elderly or renally impaired, are sitting ducks. This needs to be in every EHR alert system.
Brandon Boyd
January 1, 2026 AT 09:55Hey-if you’re on an antipsychotic and your doc hands you Reglan, say NO. Not ‘maybe,’ not ‘I’ll ask my pharmacist.’ Just say NO. Then ask for Zofran. It’s not hard. Ondansetron works just as well, no brain-stopping side effects. You’re not being difficult-you’re being alive. Your body doesn’t need two dopamine blockers. It needs one less problem. Switch it. Now.
Branden Temew
January 2, 2026 AT 02:35So let me get this straight: we’ve got a drug that’s been known to kill since the 80s, still prescribed like it’s Advil, because it’s cheap and ‘everyone knows it’s safe’? And the medical system’s response is… silence? Fascinating. We’ll happily warn people about vaping or sugar, but when it comes to polypharmacy carnage? Eh, ‘they didn’t read the label.’ Classic. The real NMS here is the system’s refusal to learn.
Frank SSS
January 2, 2026 AT 23:40Bro, I’ve been on risperidone for 5 years and my GI doc gave me Reglan for ‘bloating.’ I didn’t think twice. Then I started sweating like a sauna and couldn’t move my neck. ER said NMS. ICU for 4 days. They didn’t even ask about my meds. I’m alive. But I almost wasn’t. Now I carry a card in my wallet: ‘DO NOT GIVE METOCLOPRAMIDE.’ If you’re on an antipsychotic-do the same. Don’t wait for a near-death experience.
Paul Huppert
January 4, 2026 AT 12:21Thanks for laying this out so clearly. I’ve got a friend on olanzapine who was prescribed Reglan for nausea after chemo. I didn’t know enough to stop them-but now I do. I’m going to send them this. No one should have to learn this the hard way. Simple question: ‘Is this safe with my antipsychotic?’ should be automatic. It’s not. And that’s terrifying.
Bennett Ryynanen
January 6, 2026 AT 05:23THIS IS WHY PEOPLE DIE. I work in pharmacy. I’ve seen this combo go through 3 different prescribers before anyone caught it. One guy coded in the parking lot after filling his script. The pharmacist missed it because the antipsychotic was from a psych clinic and the metoclopramide was from a GI doc. No one talked. No one checked. We need mandatory EHR alerts. Not ‘suggestions.’ Alerts. Red flags. Loud ones.
linda permata sari
January 7, 2026 AT 21:42OMG I just read this and I’m shaking. My mom was on haloperidol and got Reglan for ‘stomach issues’-she ended up in a coma for 3 weeks. We didn’t know why. Now I know. This isn’t just medical advice-it’s a life-or-death manifesto. I’m sharing this with every family member. Everyone needs to know. 💔🔥
Hanna Spittel
January 9, 2026 AT 02:19CONSPIRACY? Nah. Just BIG PHARMA. Reglan is cheap. Zofran? $$$$. So they let doctors keep prescribing it. And patients? They don’t know. 😒💊 #ReglanKills #FDAWarningIgnored
Brady K.
January 10, 2026 AT 05:28Let’s cut through the jargon: metoclopramide + antipsychotic = dopamine suicide pact. The FDA says ‘avoid.’ Doctors say ‘it’s fine.’ Patients say ‘I felt fine for weeks.’ Then-bam. Rigidity. Fever. Kidney failure. NMS doesn’t ask if you’re ‘low risk.’ It doesn’t care if you’re ‘on an atypical.’ It just kills. And the fact that this still happens? That’s not negligence. That’s systemic malpractice. Someone’s getting paid to keep this going.
Kayla Kliphardt
January 10, 2026 AT 14:25I’m a nurse, and I’ve seen this happen twice. Both times, the patient was elderly. Both times, the metoclopramide was ordered by a non-psychiatrist who didn’t realize it was a dopamine blocker. We caught it before full NMS-but the muscle rigidity was already there. We need better interdepartmental communication. And maybe a mandatory CME module on this. It’s not rare. It’s preventable.
John Chapman
January 11, 2026 AT 02:54Just had to comment-this is the kind of post that saves lives. I’m passing this to my dad’s psych team. He’s on quetiapine and was getting Reglan for nausea. I stopped it cold and got him on Zofran. He’s fine now. Don’t wait. If you’re on an antipsychotic, don’t take metoclopramide. Period. 🙏💊
Jenny Salmingo
January 11, 2026 AT 20:44I didn’t know this was a thing. Now I do. My aunt is on risperidone and just started Reglan. I’m calling her doctor tomorrow. Thank you for sharing this. So important.