NSAID Risk Calculator
Assess Your NSAID Safety Risk
Answer these questions to determine your risk level of NSAID-related gastrointestinal bleeding. Based on the American College of Gastroenterology guidelines from the article.
Enter your information to see your risk level
Every year, millions of people reach for ibuprofen, naproxen, or diclofenac to ease joint pain, headaches, or backaches. These are NSAIDs-non-steroidal anti-inflammatory drugs-and they work. But for many, especially those over 65 or with a history of stomach issues, these pills come with a hidden danger: gastrointestinal bleeding.
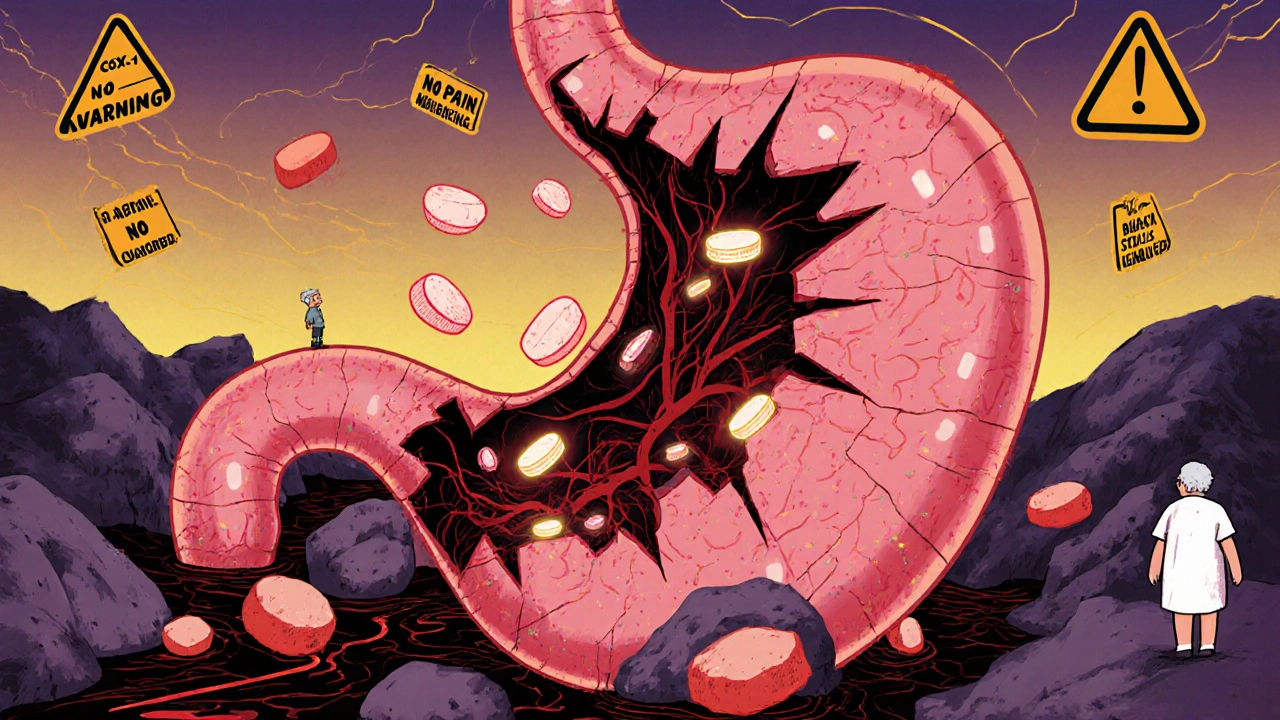
How NSAIDs Damage the Gut
NSAIDs block enzymes called COX-1 and COX-2. COX-2 causes pain and swelling, which is why these drugs help with arthritis or sprains. But COX-1 protects the stomach lining by making mucus and blood flow that keep it from getting eaten away by acid. When NSAIDs shut down COX-1, that protection disappears. The result? Erosions, ulcers, and sometimes life-threatening bleeding.You don’t need a diagnosed peptic ulcer to bleed. Studies show that 86% of people with NSAID-related lower GI bleeding never had a known ulcer. The damage can be silent-slow, steady blood loss leading to iron deficiency anemia. One patient in Liverpool, a 79-year-old woman, ended up in hospital needing three blood transfusions after months of fatigue and pale skin. Her doctor only found the cause after checking her NSAID use. She’d been taking naproxen daily for knee pain, never telling her GP about the dark stools she’d ignored.
Not All NSAIDs Are Equal
Some NSAIDs are riskier than others. Non-selective ones like ibuprofen, naproxen, and diclofenac hit both COX enzymes. That means more pain relief-but also more stomach damage. A 2000 Lancet study found that celecoxib, a COX-2 selective inhibitor, cut complicated ulcer rates by half compared to ibuprofen. But here’s the catch: COX-2 inhibitors like celecoxib and rofecoxib (now pulled from the market) raise heart attack risk. The APPROVe trial showed rofecoxib doubled the chance of heart attack after 18 months.So it’s not about picking the "safest" NSAID-it’s about matching the drug to the person. For someone with heart disease, even a low-dose NSAID can be dangerous. For someone with a history of ulcers, avoiding NSAIDs altogether might be the best move.
Who’s at Highest Risk?
It’s not just age. The American College of Gastroenterology lays out clear risk factors:- Age over 70 (risk doubles per decade)
- History of peptic ulcer or GI bleeding
- Taking blood thinners like warfarin or apixaban
- Using corticosteroids (like prednisone)
- Taking more than one NSAID at once
- High doses-over 1,200 mg of ibuprofen daily
- Chronic conditions like kidney disease or heart failure
If you have two or more of these, your risk jumps. A 2017 Cochrane review found that people with two risk factors had a 10 times higher chance of bleeding than someone with none. And here’s the scary part: many people don’t even know they’re at risk. A 2022 survey on HealthUnlocked showed 63% of NSAID users had stomach symptoms-bloating, nausea, black stools-but only 37% told their doctor.
How to Protect Your Stomach
If you need an NSAID and you’re at risk, you don’t have to go without pain relief. Protection works.Proton pump inhibitors (PPIs)-like omeprazole, pantoprazole, or esomeprazole-are the gold standard. A 2017 Cochrane review of over 13,000 patients found PPIs cut NSAID-related ulcers by 75%. That’s not a small benefit. That’s life-saving. For someone who’s had a bleed before, the American College of Gastroenterology says combining a COX-2 inhibitor with a PPI is the strongest protection. The number needed to treat is just 16-meaning for every 16 high-risk patients on this combo, one serious ulcer is prevented over 12 weeks.
Misoprostol also works, reducing ulcers by 50-75%, but it causes diarrhea in up to 20% of users and isn’t safe in pregnancy. It’s rarely used today.
There’s also a newer option: Vimovo, a pill that combines naproxen with esomeprazole in one tablet. The 2022 PRECISION-2 trial showed it slashed ulcer complications from 25.6% to just 7.3% compared to plain naproxen. It’s not cheap, but for high-risk patients, it’s a game-changer.
What About Over-the-Counter NSAIDs?
People think OTC means safe. It doesn’t. A 2021 review found 26% of people take OTC NSAIDs at doses higher than recommended-and most never mention it to their doctor. That’s a huge blind spot. A 40-year-old taking two ibuprofen tablets four times a day for back pain is hitting 1,200 mg daily-the danger zone. No prescription needed, no warning label loud enough.And the damage isn’t always obvious. Iron deficiency anemia from slow, hidden bleeding is common in older adults. It’s mistaken for aging, fatigue, or poor diet. One Reddit user shared how their 78-year-old mother was diagnosed with severe anemia after months of feeling "just tired." The cause? Daily ibuprofen for osteoarthritis. No stomach pain. No black stools. Just low hemoglobin.
Real Choices, Real Trade-Offs
Let’s say you’re 72, have arthritis, and had a stomach ulcer five years ago. You need pain relief. Here’s your realistic path:- Stop NSAIDs if possible. Try acetaminophen (paracetamol) first. It doesn’t hurt the stomach.
- If that doesn’t work, ask your doctor about a COX-2 inhibitor like celecoxib.
- Take it with a daily PPI like omeprazole 20 mg.
- Use the lowest dose that helps. Don’t take more just because you "feel like it."
- Get checked for anemia yearly. A simple blood test catches bleeding before it’s an emergency.
For someone younger, with no history of ulcers or heart disease, occasional ibuprofen might be fine. But if you’re using it every day for three months straight, that’s not occasional. That’s chronic use-and that’s when risk spikes.
The Bigger Picture
NSAIDs cause about 107,000 hospitalizations and 16,500 deaths each year in the U.S. alone. The cost? Over $2 billion. Globally, the market is worth $11.3 billion. That’s a lot of money spent on drugs that are both helpful and harmful.Regulators know this. Since 2005, the FDA has required black box warnings on all NSAID labels-clear, bold text saying they can cause ulcers and bleeding. But warnings don’t change behavior. Patients don’t read them. Pharmacists don’t always explain them. Doctors are rushed.
The solution isn’t banning NSAIDs. It’s smarter use. The American College of Rheumatology’s 2023 guidelines say it clearly: For one risk factor, use the lowest NSAID dose for the shortest time. For two or more risk factors-don’t start NSAIDs without gastroprotection.
What You Can Do Today
If you’re taking NSAIDs regularly:- Ask your doctor: "Do I have any risk factors for stomach bleeding?"
- Ask: "Should I be on a PPI too?"
- Ask: "Is there a non-NSAID option for my pain?"
- Watch for symptoms: black or tarry stools, vomiting blood, unexplained fatigue, dizziness.
- Don’t ignore "minor" stomach upset. It might be the first sign of something worse.
And if you’re helping an older relative: check their medicine cabinet. Are they taking multiple painkillers? Do they have unexplained anemia? Ask questions. You might prevent a hospital trip.
Can I take ibuprofen if I’ve had a stomach ulcer before?
If you’ve had a peptic ulcer or GI bleed, you should avoid NSAIDs like ibuprofen unless absolutely necessary. If you must take one, combine it with a proton pump inhibitor (PPI) like omeprazole. The safest option is a COX-2 inhibitor (like celecoxib) with a PPI. Never restart an NSAID after a bleed without consulting your doctor.
Do all NSAIDs cause bleeding?
All NSAIDs carry some risk, but the level varies. Non-selective NSAIDs like naproxen and diclofenac are the most likely to cause bleeding. COX-2 inhibitors like celecoxib are safer for the stomach-but carry higher heart risks. Even low-dose aspirin, which is also an NSAID, increases bleeding risk. No NSAID is completely safe for the gut.
How do I know if I’m bleeding from NSAIDs?
Signs include black, tarry stools (melena), vomiting blood or material that looks like coffee grounds, extreme fatigue, dizziness, or shortness of breath. Sometimes, there are no symptoms at all-just low iron levels from slow, hidden bleeding. A simple blood test can detect anemia before it becomes serious. If you’re on NSAIDs and feel unusually tired, get checked.
Is it safe to take NSAIDs with blood thinners?
No, it’s very risky. Combining NSAIDs with blood thinners like warfarin, apixaban, or rivaroxaban increases bleeding risk by more than double. If you’re on a blood thinner and need pain relief, acetaminophen (paracetamol) is the preferred option. If you must use an NSAID, do so only under close medical supervision with a PPI.
Can I stop NSAIDs cold turkey?
For most people, yes. Stopping NSAIDs won’t cause withdrawal. But if you’ve been using them daily for chronic pain, stopping suddenly might make your pain worse. Talk to your doctor first. They can help you switch to safer alternatives like physical therapy, acetaminophen, or other non-NSAID pain management options.
What Comes Next?
New drugs are coming. Naproxcinod, a type of CINOD (COX-inhibiting nitric oxide donor), showed 50% fewer ulcers than naproxen in trials. But these aren’t on the market yet. For now, the best tools we have are awareness, risk assessment, and PPIs.The bottom line? NSAIDs aren’t evil. They’re powerful tools. But like a chainsaw, they need respect. Use them only when needed, at the lowest dose, and protect your stomach if you’re at risk. Your gut will thank you-and you might avoid a hospital bed you never saw coming.




Chrisna Bronkhorst
November 11, 2025 AT 19:10Eve Miller
November 13, 2025 AT 01:48Amie Wilde
November 13, 2025 AT 16:48Elizabeth Buján
November 15, 2025 AT 07:11Andrew Forthmuller
November 16, 2025 AT 05:08vanessa k
November 17, 2025 AT 16:05manish kumar
November 18, 2025 AT 22:55Nicole M
November 19, 2025 AT 20:36Arpita Shukla
November 21, 2025 AT 13:26Benjamin Stöffler
November 22, 2025 AT 06:45Mark Rutkowski
November 22, 2025 AT 16:41Ryan Everhart
November 23, 2025 AT 13:06David Barry
November 24, 2025 AT 05:05Alyssa Lopez
November 26, 2025 AT 00:25Alex Ramos
November 27, 2025 AT 02:26