More than half of adults over 65 in the U.S. are taking five or more medications every day. That’s not just common-it’s dangerous. Polypharmacy, the term for taking five or more drugs at once, isn’t a treatment plan. It’s a symptom of a broken system. And for older adults, it’s one of the leading causes of falls, confusion, hospital stays, and even death.
Why Polypharmacy Is a Silent Crisis
It starts with good intentions. An older person sees a cardiologist for high blood pressure, a rheumatologist for arthritis, a neurologist for sleep issues, a gastroenterologist for acid reflux, and their primary care doctor for diabetes. Each specialist prescribes what they think is best. No one steps back to look at the full picture.
By the time they get home, they’re juggling 10 pills at different times of day. Some are for conditions they no longer have. Others interact badly with each other. One study found that 40% of older adults globally are taking medications that do more harm than good. In the U.S. alone, polypharmacy contributes to 10% of all hospital admissions in people over 65-and costs over $30 billion a year.
It’s not just the number of pills. It’s what’s in them. Benzodiazepines for sleep? They increase fall risk by 50%. NSAIDs for joint pain? They can cause dangerous stomach bleeding. Anticholinergics for overactive bladder? Linked to a 50% higher chance of dementia over seven years. These aren’t rare side effects. They’re predictable outcomes.
How Aging Changes the Way Medications Work
Your body doesn’t process drugs the same way at 75 as it did at 45. Liver function drops by 30-50% after age 80. Kidneys clear drugs more slowly-about 1% less each year after 40. That means medications stay in your system longer. A dose that was safe at 60 can become toxic at 75.
Think of it like pouring water into a cup that’s shrinking. The same amount of medicine that fit safely before now overflows. That’s why older adults are 7 times more likely to be hospitalized for adverse drug reactions than younger people. It’s not that they’re taking too many pills. It’s that their bodies can’t handle what they’re already taking.
The Big Three: Most Dangerous Medications for Seniors
The American Geriatrics Society’s Beers Criteria lists 56 medications that should be avoided or used with extreme caution in people over 65. Three stand out as especially risky:
- Benzodiazepines (like diazepam, lorazepam): Used for anxiety or sleep, but they cause dizziness, confusion, and falls. One in three seniors on these drugs ends up in the ER after a fall.
- NSAIDs (like ibuprofen, naproxen): Common for arthritis, but they raise the risk of internal bleeding by 2.5 times. Many seniors don’t realize they’re taking these-some are in over-the-counter combo pills.
- Anticholinergics (like diphenhydramine, oxybutynin): Found in allergy meds, sleep aids, and bladder pills. They block a key brain chemical, leading to memory problems, constipation, and urinary retention. Long-term use raises dementia risk by 50%.
Many seniors are still on these drugs because no one ever asked if they still needed them. That’s the problem. Medications are often prescribed and never reviewed again.
Deprescribing: The Missing Step in Care
There’s no medical term for stopping a drug you don’t need. But there should be. That’s what deprescribing is-the careful, planned reduction or elimination of medications that no longer benefit the patient.
It’s not about cutting pills. It’s about rethinking goals. At 90, the goal isn’t to hit a perfect blood pressure number. It’s to stay out of the hospital, walk without falling, and remember your grandchildren’s names.
Studies show that when deprescribing is done right, it reduces adverse drug events by 22% and hospital admissions by 17%. One program at UCI Health found an average of 4.2 inappropriate medications per patient during a full review. After stopping those, patients reported better sleep, clearer thinking, and fewer trips to the bathroom at night.
But deprescribing doesn’t happen unless someone asks: Why are you still taking this?

How to Take Control of Your Medications
You don’t need to be a doctor to manage your meds. You just need to be organized and speak up.
- Do a brown bag review. Every six months, take every pill, capsule, patch, and supplement you take-including vitamins, herbal teas, and OTC painkillers-and put them in a bag. Bring them to your doctor. Most people bring 2-3 extra meds they didn’t even realize they were still taking.
- Ask the three questions. At every appointment, ask: What is this for? Do I still need it? What happens if I stop it? If your doctor can’t answer clearly, it’s a red flag.
- Know your pharmacist. Pharmacists are medication detectives. They see all your prescriptions across all doctors. Ask them to check for interactions. Many pharmacies offer free medication reviews.
- Use one pharmacy. If you use multiple pharmacies, your drug interactions won’t be flagged. Stick to one. It’s the only way the system can warn you.
- Track your symptoms. Keep a simple log: When did you start this pill? Did you feel worse after? Did your balance change? Did you get dizzy? Write it down. Bring it to your next visit.
When Multiple Doctors Are the Problem
One in three seniors sees three or more specialists. Each one writes a prescription. Few talk to each other. The result? Duplicate drugs, conflicting advice, and dangerous overlaps.
For example: one doctor prescribes a blood thinner. Another prescribes an NSAID for pain. Together, they increase bleeding risk by 5 times. No one connected the dots.
The fix? Appoint one person as your medication captain. Usually, that’s your primary care doctor. But if they’re overwhelmed, ask for a pharmacist-led medication therapy management (MTM) program. Medicare covers it. It’s free. And it cuts hospital readmissions by 24%.
Cost Is a Hidden Danger
One in four seniors skips doses because they can’t afford their meds. That’s not adherence-it’s survival. But skipping pills can be just as dangerous as taking too many.
Instead of cutting pills, ask: Is there a generic? A lower-cost alternative? A program that helps? Many drugmakers offer patient assistance programs. Pharmacists know them. Ask.
Also, check if you’re paying for drugs you don’t need. A 2022 study found that 30% of seniors on Medicare Part D were paying for medications that were no longer clinically indicated. Deprescribing saved them $1,049 per person annually.
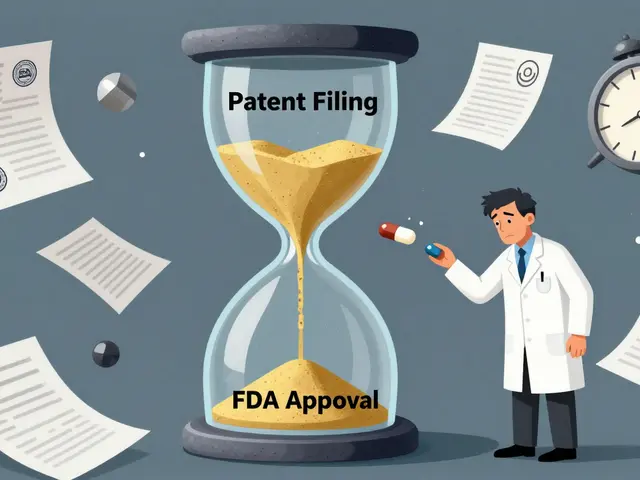
The Future: Personalized Medicine for Seniors
The next big shift isn’t adding more drugs-it’s removing the wrong ones. New tools are emerging to help.
The FDA-approved MedWise platform uses genetic data to predict how your body will react to specific drugs. In trials, it cut adverse events by 41%. The Centers for Medicare & Medicaid Services launched a $15 million initiative in early 2023 to train doctors in deprescribing. And researchers are now studying how biological age-not calendar age-should guide prescribing.
Imagine a future where your medication list isn’t based on what’s been added over 20 years, but on what your body can still handle today. That’s the goal.
What You Can Do Today
You don’t need to wait for a new technology or a policy change. Start now.
- Make a list of every medication you take, including doses and times.
- Bring it to your next doctor visit. Don’t wait for a ‘medication review’-ask for one.
- Ask if any of your meds can be stopped, lowered, or switched.
- If you feel worse after starting a new pill, say so. Don’t assume it’s just ‘getting older.’
Polypharmacy isn’t inevitable. It’s a choice. And you have the power to change it.
What is considered polypharmacy in elderly patients?
Polypharmacy is defined as the regular use of five or more medications at the same time. It’s not just about the number-it’s about whether those medications are still necessary, safe, and aligned with the patient’s current health goals. For older adults, even four medications can be risky if they interact or are inappropriate for their age.
Can stopping medications be dangerous?
Stopping some medications suddenly can be dangerous-like blood pressure or seizure drugs. But continuing unnecessary ones is often more dangerous. Deprescribing is done slowly and under medical supervision. The goal is to remove drugs that no longer help or that cause more harm than benefit. Studies show that when done properly, stopping these meds improves safety and quality of life.
Are over-the-counter drugs part of the problem?
Absolutely. Many seniors take OTC painkillers, sleep aids, or antacids daily without realizing they’re medications. Diphenhydramine (found in Benadryl and many sleep aids) is an anticholinergic linked to dementia. Ibuprofen can cause stomach bleeds. These are not harmless. Always include them in your brown bag review.
How often should seniors have a medication review?
At least once a year-but ideally after every hospital stay, ER visit, or change in health. Medication needs change as you age. A pill that helped at 70 might be harmful at 80. Every transition in care is a chance to reset your list.
Can pharmacists help with polypharmacy?
Yes. Pharmacists are trained to spot drug interactions, duplicate therapies, and inappropriate prescriptions. Medicare offers free Medication Therapy Management (MTM) services for eligible beneficiaries. Ask your pharmacist to run a full review. They can also help you simplify your schedule and find lower-cost options.
What are the signs that medications are causing problems?
New dizziness, confusion, memory lapses, falls, constipation, urinary problems, or sudden fatigue can all be signs of medication side effects-not just aging. If symptoms started after adding a new drug, that’s a red flag. Don’t ignore them. Bring your medication list to your doctor and say, ‘Could this be from my pills?’
Next Steps for Families and Caregivers
If you’re helping an older loved one manage their meds:
- Help them keep a written list-and update it every time a new prescription comes in.
- Go with them to appointments. Doctors often don’t notice what’s missing. You might.
- Don’t assume they understand why they’re taking each pill. Ask them to explain it back to you.
- Watch for changes in behavior, appetite, or mobility. These can be early signs of drug toxicity.
- Push for a pharmacist review. It’s free under Medicare and often overlooked.
Managing multiple medications isn’t about taking more. It’s about taking less-wisely. The goal isn’t to live longer with a pill bottle. It’s to live better with fewer pills-and more freedom.




Tim Goodfellow
December 18, 2025 AT 20:10Man, this post hit like a freight train. I’ve seen my grandma juggle 12 pills a day-some for stuff she’s had for 20 years, some she forgot she even started. And no one ever asked if she still needed them. It’s not care-it’s autopilot. We treat elders like walking pharmacy inventories instead of people.
Alex Curran
December 19, 2025 AT 06:01Deprescribing isn’t just smart-it’s radical. Most docs get paid to add meds, not remove them. No incentive to stop. But pharmacists? We’re the ones catching the duplicates, the interactions, the OTC nightmares. I’ve seen diphenhydramine cause more confusion than dementia. Stop calling it ‘just aging.’ It’s iatrogenic.
Sarah McQuillan
December 20, 2025 AT 18:35Why are we letting pharmaceutical companies dictate how old people live? These drugs aren’t miracles-they’re profit margins. And the system rewards prescribing, not pausing. You think this is about health? It’s about revenue. 30 billion a year? That’s not a cost. That’s a business model.
Kelly Mulder
December 22, 2025 AT 03:35It is, quite frankly, an abomination that geriatric pharmacology remains so woefully underdeveloped in clinical training. The Beers Criteria are not suggestions-they are clinical imperatives, yet they are routinely ignored by specialists who operate in silos of ignorance. One must wonder whether the medical-industrial complex has intentionally obfuscated deprescribing as a concept to preserve revenue streams.
Dominic Suyo
December 23, 2025 AT 12:21Oh wow. Another sanctimonious rant about pills. Let me guess-you think every senior on a statin is being poisoned? Wake up. Some of these people would be dead without their meds. You’re romanticizing risk. Not everyone wants to ‘live better with fewer pills’-some want to live at all.
Alisa Silvia Bila
December 24, 2025 AT 15:29I love how this post doesn’t just list problems-it gives real steps. Brown bag review? Yes. One pharmacy? Yes. Asking ‘what happens if I stop it?’? That’s the golden question. My aunt did this last year. Stopped three meds. Now she sleeps through the night. No more dizziness. No more confusion. Just her.
Nina Stacey
December 25, 2025 AT 13:59so i just took my 82 year old mom to the dr and she had 11 meds on her list and i was like wow this is insane and then the dr said oh this one is for your mom's high blood pressure and i said but she's been on it for 15 years and she's not even hypertensive anymore and he just nodded and wrote another script for a new antidepressant and i was like wait what
Jedidiah Massey
December 26, 2025 AT 23:12Let’s be clear: polypharmacy is a biomarker of systemic failure. The cognitive load of managing multiple regimens exceeds the executive function capacity of most elderly patients. Add in pharmacokinetic decline, and you’ve got a perfect storm of iatrogenic morbidity. The solution? MTM. It’s evidence-based. It’s reimbursable. And it’s still underutilized because the system is broken. End of story.
Takeysha Turnquest
December 27, 2025 AT 00:49we are taught to fear death so we chase pills instead of peace
we are told to fix everything so we forget to feel
we are sold medicine as hope so we stop asking what we are really healing
Marsha Jentzsch
December 27, 2025 AT 06:47Did you know that 78% of seniors on anticholinergics are being secretly poisoned by Big Pharma? They know these drugs cause dementia. They’ve had the studies since 2003. But they keep selling them because old people don’t vote enough. My cousin died after taking Benadryl for a cold. They called it ‘natural causes.’ It was murder.
anthony funes gomez
December 28, 2025 AT 11:29It’s not about the number of pills. It’s about the number of assumptions. Assumption: the patient understands. Assumption: the doctor communicates. Assumption: the system coordinates. Assumption: aging equals decline. Assumption: more is better. Assumption: compliance is the goal. Assumption: death is failure. Assumption: life is measured in lab values. Assumption: the body is a machine. Assumption: the soul doesn’t matter. Assumption: we’ve got this. We don’t. We never did.
James Stearns
December 29, 2025 AT 04:20As a physician with over 25 years of clinical experience, I must emphasize that the notion of deprescribing as a routine practice remains highly controversial within academic geriatrics. While the Beers Criteria are useful, they are not universally applicable. Each patient’s clinical context must be evaluated individually. To generalize is to endanger.
Kevin Motta Top
December 29, 2025 AT 08:25My dad’s pharmacist caught a dangerous interaction between his blood pressure med and a supplement he was taking. Free review. Took 2 pills off his list. He sleeps better. Walks better. Talks better. You don’t need a PhD to fix this. You just need to ask.
Edington Renwick
December 30, 2025 AT 22:11Everyone’s so obsessed with cutting pills. But what about the ones who actually need them? What about the guy on 8 meds because he’s got diabetes, CHF, AFib, and dementia? You think taking one away will help? You’re not helping. You’re playing doctor. Real medicine isn’t a checklist. It’s a balancing act. And you’re just making it worse.
Janelle Moore
January 1, 2026 AT 14:56They’re putting microchips in the pills to track us. That’s why they won’t let you stop anything. The government wants to know who’s still alive. That’s why they push meds on seniors. It’s not health. It’s surveillance.