If you’ve ever lain awake at night with an unbearable urge to move your legs-like something’s crawling under your skin, or your muscles are twitching with electric energy-you’re not alone. Restless Legs Syndrome (RLS), also called Willis-Ekbom Disease, affects 5 to 10% of adults in the U.S. and Europe. And for many, the real culprit isn’t stress or bad sleep habits-it’s low iron in the brain, even when your blood tests look "normal."
Why Iron Matters More Than You Think
RLS isn’t just a twitchy leg problem. It’s a neurological disorder tied to how your brain uses iron. Your body might have enough iron in your blood, but if your brain isn’t getting it, your nerves misfire. This happens because iron is essential for producing dopamine, the brain chemical that helps control movement. When dopamine drops, your legs feel restless.
The key marker doctors look at isn’t serum iron or hemoglobin-it’s ferritin. Ferritin is the protein that stores iron in your body. And for RLS, the cutoff isn’t the standard "normal" range of 12-300 ng/mL. It’s much stricter.
Multiple major medical groups-including the American Academy of Neurology, the American Academy of Sleep Medicine, and the European Restless Legs Syndrome Study Group-agree: if your ferritin is below 50 ng/mL, you’re at high risk for moderate to severe RLS. Studies show people with ferritin under 50 are three times more likely to have intense nighttime symptoms than those above that level.
The 50 ng/mL Threshold: Why It’s Not a Mistake
Many doctors still think "normal" ferritin means "fine." But that’s outdated. A landmark 1997 study by Dr. Richard Allen and colleagues found RLS patients had an average ferritin of 28.4 ng/mL, while healthy people averaged 62.1 ng/mL. Since then, over 20 clinical trials have confirmed that raising ferritin above 50 ng/mL leads to real symptom improvement.
Even more telling: patients with ferritin between 50 and 75 ng/mL still respond to iron therapy. One study in the European Journal of Neurology found 35% of patients saw at least half their symptoms vanish after iron supplementation-even though their levels were "within range."
That’s why leading sleep specialists now treat RLS based on ferritin, not just symptoms. If you have RLS and ferritin is below 75 ng/mL, iron therapy is recommended as a first step-before you even try dopamine drugs.
Oral Iron: What Works and What Doesn’t
So how do you raise ferritin? Most people start with oral iron supplements. The most common form is ferrous sulfate-325 mg tablets, which give you 65 mg of elemental iron. That’s a lot. But here’s the catch: your gut doesn’t absorb it well, especially if you take it with food.
For best results:
- Take it on an empty stomach, 1 hour before or 2 hours after meals
- Pair it with 100-200 mg of vitamin C (like a glass of orange juice or a supplement) to boost absorption
- Avoid calcium, antacids, or coffee within 2 hours-these block iron uptake
But here’s the problem: 25-30% of people can’t tolerate oral iron. Stomach pain, nausea, constipation, or diarrhea are common. Some give up after a few days.
There’s a workaround: try alternate-day dosing. Instead of taking iron every day, take it every other day. Studies in Blood Advances show this keeps ferritin rising just as effectively-while cutting side effects by nearly half.
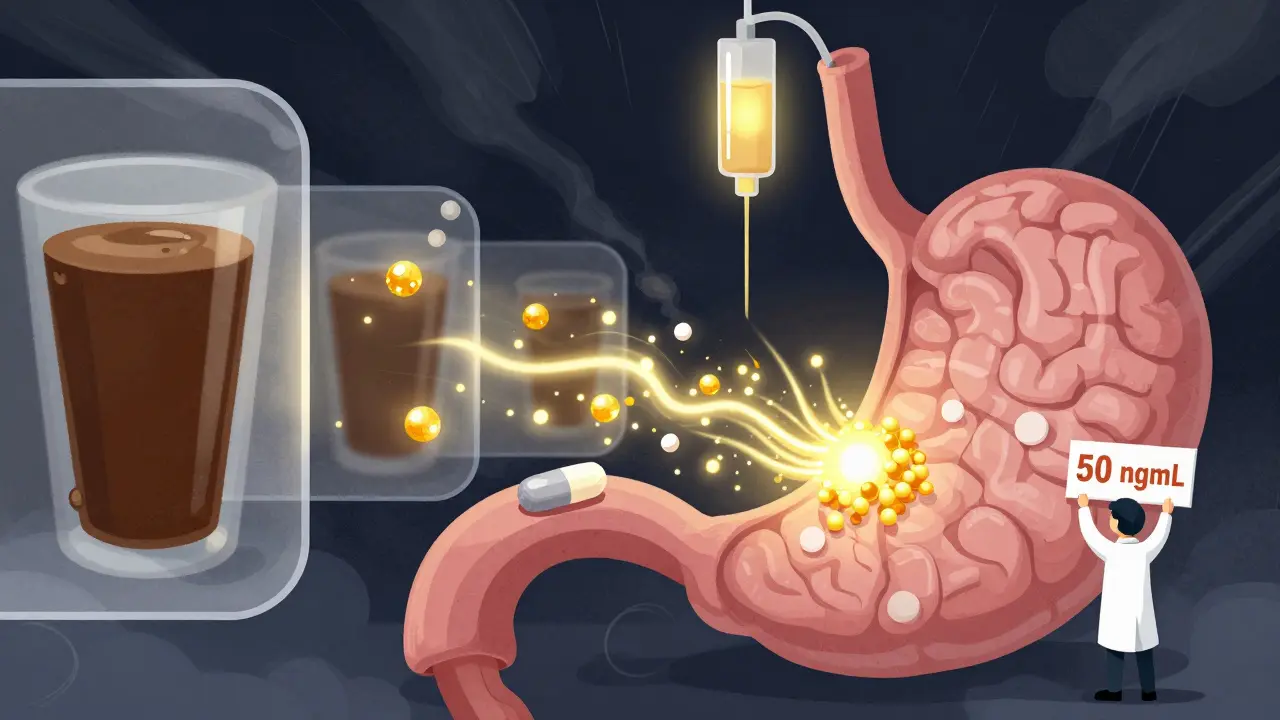
When Oral Iron Fails: The Power of IV Iron
If you’ve tried oral iron for 8-12 weeks and your ferritin is still under 50 ng/mL, or you can’t tolerate it at all, it’s time to consider intravenous (IV) iron.
IV iron-like ferric carboxymaltose-delivers iron directly into your bloodstream. One single infusion of 1000 mg can raise your ferritin by an average of 127 ng/mL in just 6 weeks. That’s faster than taking pills for 6 months.
And the results? In a 2021 trial, 68% of patients saw major RLS improvement after one IV dose. Symptoms stayed under control for up to 2 years in 65% of patients. Compare that to dopamine drugs, where 60-80% develop worsening symptoms over time (called augmentation).
IV iron isn’t perfect-it’s more expensive, requires a clinic visit, and can cause temporary headaches or dizziness. But for those who don’t respond to pills, it’s often life-changing.
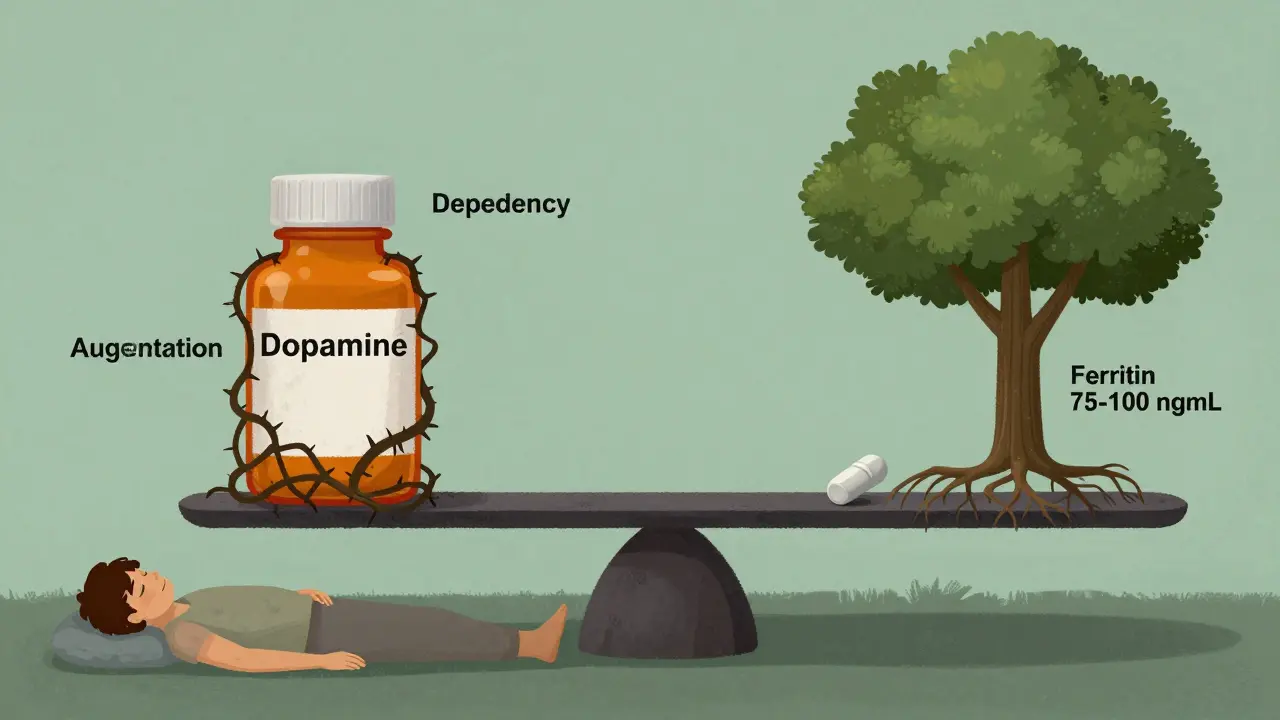
Iron vs. Dopamine Drugs: The Real Trade-Off
Many doctors still start RLS patients on dopamine agonists like pramipexole or ropinirole. They work fast-sometimes in days. But they come with a hidden cost.
Augmentation happens when the medication makes RLS worse: symptoms start earlier in the day, spread to your arms, or become more intense. After 10 years on these drugs, up to 70% of severe RLS patients develop augmentation. Once it happens, stopping the drug is hard-and symptoms can be worse than before.
Iron therapy? Almost no risk of augmentation. No dependency. No withdrawal. Just a slow, steady fix to the root cause.
Cost-wise, iron wins too. A year of oral iron costs $185-$350. A year of dopamine drugs? $2,400-$4,800. And IV iron? One infusion costs about $1,200, but often lasts 1-2 years. That’s a savings of over $2,000 per year.
What About Diet? Can You Eat Your Way Out of RLS?
Some people think eating more red meat or spinach will fix RLS. It won’t.
Heme iron from red meat is better absorbed than plant iron-but you’d need to eat 3-4 servings of steak daily to match the iron in one 325 mg ferrous sulfate pill. And even then, absorption varies wildly based on genetics, gut health, and inflammation.
Spinach? It’s full of iron, but it’s non-heme iron, blocked by oxalates and phytates. You’d need to eat 10 cups of cooked spinach to get 10 mg of absorbable iron. Not realistic.
Diet alone won’t fix RLS. But it can support therapy. Pair your iron supplement with vitamin C-rich foods: bell peppers, citrus, strawberries, broccoli. Avoid tea and coffee with meals-they inhibit iron absorption.
Testing and Monitoring: What Your Doctor Should Check
If you suspect RLS, ask for these tests:
- Serum ferritin-the most important one
- Serum iron
- Total iron-binding capacity (TIBC)
- Transferrin saturation (calculated from serum iron and TIBC)
If ferritin is below 75 ng/mL, you’re a candidate for iron therapy-even if other numbers look okay.
After starting iron, retest ferritin at 8-12 weeks. Target: 75-100 ng/mL. That’s the sweet spot for most RLS patients. Going higher than 100 isn’t necessary and could increase oxidative stress.
Some newer research suggests checking hepcidin-a hormone that blocks iron absorption. High hepcidin (above 10 ng/mL) means your body is actively preventing iron from reaching your brain, even if you’re taking supplements. If your hepcidin is high and ferritin is low, IV iron is likely your best bet.
What’s Next? New Treatments on the Horizon
Researchers are testing new iron forms that are easier on the stomach and better absorbed:
- Ferric maltol: Already approved in Europe, it’s gentler on the gut and has 40% better absorption than ferrous sulfate
- Liposomal iron: Iron wrapped in fat bubbles that bypass the gut entirely-early trials show fewer side effects and faster ferritin rise
The American Academy of Sleep Medicine is expected to update its guidelines in mid-2024 to recommend IV iron as a first-line option for RLS patients with ferritin under 75 ng/mL. That’s a big shift-from treating symptoms to treating the cause.
For now, the message is clear: if you have restless legs, get your ferritin checked. Don’t wait for your doctor to bring it up. If it’s under 50, start iron therapy. If it’s under 75 and symptoms are bad, talk to your doctor about IV iron. This isn’t a quick fix-it’s a long-term solution that could keep you off powerful drugs forever.
Can low iron cause restless legs even if my blood count is normal?
Yes. Restless Legs Syndrome is linked to low iron in the brain, not low blood iron. You can have normal hemoglobin and still have ferritin below 50 ng/mL, which is enough to trigger RLS symptoms. That’s why ferritin-not hemoglobin-is the key test.
How long does it take for iron supplements to work for RLS?
It usually takes 4 to 8 weeks to see improvement with oral iron. Some people notice changes in 2-3 weeks, but full results take longer. IV iron works faster-symptoms often improve within 2 weeks. Patience is key; this isn’t a pill that works overnight.
Can I take iron with my other medications?
Avoid taking iron with calcium supplements, antacids, thyroid meds, or antibiotics like tetracycline-they block absorption. Take iron at least 2 hours before or after these drugs. Vitamin C helps, so take it with your iron. Always check with your doctor or pharmacist if you’re on multiple medications.
Is it dangerous to take too much iron?
Yes. Too much iron can damage your liver and increase oxidative stress. Don’t take iron unless your ferritin is low. Don’t exceed 65 mg of elemental iron daily unless under medical supervision. Iron overload is rare in RLS patients because the goal is to reach 75-100 ng/mL-not to go higher. Regular blood tests prevent this risk.
Should I avoid dopamine drugs completely if I have low ferritin?
Not necessarily-but iron should come first. If your ferritin is under 75 ng/mL, try iron therapy for 8-12 weeks before starting dopamine drugs. If symptoms improve, you may never need them. If they don’t, then dopamine meds can be added. Starting with dopamine when iron is low increases your risk of augmentation and long-term worsening.
Can I stop iron supplements once my symptoms get better?
Not right away. Once your ferritin hits 75-100 ng/mL and symptoms improve, keep taking a low dose (like 325 mg ferrous sulfate every other day) for 3-6 months to rebuild your iron stores. Then, retest ferritin. If it stays above 50, you may be able to stop. But many people need to take low-dose iron long-term to prevent relapse.



Sarah Little
January 3, 2026 AT 22:48Post-ferritin thresholds are non-negotiable in neurology now. Serum iron is a red herring-ferritin under 50 ng/mL is the biomarker that predicts RLS severity, not hemoglobin. The 1997 Allen study still holds up, and recent meta-analyses confirm IV iron’s superiority in refractory cases. If your doc says "it’s normal," they’re using 1990s guidelines. Time to push back.
innocent massawe
January 5, 2026 AT 22:32Interesting. I live in Nigeria where iron deficiency is common, but no one talks about RLS here. Maybe because we focus on anemia first. But this makes sense-brain iron ≠ blood iron. I’ll share this with my cousin who’s always tossing and turning at night. 🙏
Tru Vista
January 7, 2026 AT 01:14Oral iron is garbage. I took ferrous sulfate for 3 months, got constipated, ferritin went from 32 to 38. Zero change. IV iron? 1000mg, 2 weeks later-ferritin 94. Legs stopped screaming. Doc said "it’s off-label" but the AAN says otherwise. Also, vitamin C is non-negotiable. Skip the orange juice, take 200mg tabs.
Angela Fisher
January 7, 2026 AT 14:46They don’t want you to know this. Big Pharma doesn’t profit from $185 iron pills. That’s why they push dopamine drugs-$4k a year, lifelong dependency, augmentation guaranteed. IV iron? One shot, $1200, lasts two years. And they call it "experimental"? Lol. The FDA’s asleep. Ferritin under 75? They’re lying to you. This is a cover-up. Check your hepcidin. If it’s high, your body’s blocking iron on purpose. Who’s controlling that? Big Ag? Big Med? I’m not paranoid. I’m informed. 🧠⚠️
Neela Sharma
January 8, 2026 AT 23:54Iron isn’t just a mineral-it’s the quiet conductor of your nervous system’s symphony. When ferritin drops below 50, the dopamine orchestra goes silent and your legs start screaming for attention. IV iron isn’t a treatment-it’s a resurrection. No drugs. No addiction. Just your body remembering how to be still. I’ve seen it. My sister went from pacing at 2am to sleeping through dawn. No magic. Just science that was ignored for too long. 🌅
Shruti Badhwar
January 10, 2026 AT 01:14While the data supporting ferritin thresholds above 50 ng/mL is compelling, it is imperative to consider individual variability in iron metabolism. Genetic polymorphisms in HFE, TMPRSS6, and hepcidin regulation can significantly influence therapeutic response. Therefore, a one-size-fits-all approach may not be optimal. Personalized medicine, incorporating genetic screening and longitudinal ferritin tracking, should be prioritized in clinical practice.
Michael Burgess
January 11, 2026 AT 11:14Just had my first IV iron last week. Ferritin was 29. Now it’s 88. I slept 7 hours straight last night for the first time in 14 years. 🤯 No more midnight leg yoga. No more anxiety about bedtime. I’m not even mad about the 20-minute drip. Worth every second. Also-yes, vitamin C. Always. I chugged a whole bottle of OJ like it was my job.
Wren Hamley
January 11, 2026 AT 12:10Wait, so if ferritin’s 65 and I still have RLS, do I still need IV? The paper in Eur J Neurol said 35% improved even between 50-75. So is 75 the real cutoff or just a soft target? Also, what’s the deal with ferric maltol? Is it available in the US yet or still stuck in regulatory limbo?
Philip Leth
January 11, 2026 AT 19:53Bro, I’m from the South. We don’t do IVs unless it’s a snakebite or a bad hangover. But after reading this, I made my doctor order ferritin. 38. Two weeks of oral iron + OJ. Now I’m at 68. No more leg monsters at midnight. You don’t need a PhD to get this right. Just ask for the test. And drink the damn orange juice.