Amiloride Pregnancy Risk Calculator
Potassium Risk Assessment
Calculate your hyperkalemia risk based on current potassium levels and kidney function
Risk Assessment Results
Recommendations
- Monitor potassium levels:
- Consult your healthcare provider:
When you’re expecting a baby, every medication you take turns into a big question mark. Amiloride pregnancy concerns are no different - you need clear facts, not speculation. This guide breaks down how amiloride works, what the research says about its safety in pregnancy, and practical steps for you and your healthcare team.
What is Amiloride?
Amiloride is a potassium‑sparing diuretic that blocks epithelial sodium channels (ENaC) in the distal convoluted tubule and collecting duct. By limiting sodium reabsorption, it promotes modest water loss while retaining potassium. Doctors primarily prescribe it for hypertension, congestive heart failure, and certain forms of kidney disease where potassium loss is a concern.
How Does Amiloride Fit Into Pregnancy?
Pregnancy is a physiological state that alters fluid balance, kidney function, and hormone levels. These changes can affect how drugs behave - they may accumulate more, clear slower, or cross the placenta differently. Understanding amiloride’s pharmacokinetics during pregnancy is the first step to judging its risk.
Amiloride has a relatively short half‑life (6‑9 hours) and is excreted unchanged by the kidneys. Because the placenta is semi‑permeable to small molecules, a minimal amount can reach the fetus, but concrete data are scant.
Regulatory Classification and the Evidence Base
The Food and Drug Administration (FDA) classifies drugs for pregnancy using categories A, B, C, D, and X. Amiloride falls into Category C - animal studies have shown some adverse effects, but there are no well‑controlled human studies, and the potential benefits may justify use.
Human case reports are limited to a handful of pregnancies where amiloride was continued for severe hypertension. In most of those reports, outcomes were uneventful, but the sample size is too small to draw firm conclusions.
Key points from the literature:
- Animal studies (rat, rabbit) reported fetal growth retardation at high doses.
- No definitive teratogenic signal (birth defects) has been proven.
- Potential for maternal potassium depletion, which can affect fetal heart rhythm.
Potential Risks and Side Effects for Mom and Baby
Because amiloride spares potassium, the most common concern is hyperkalemia elevated potassium levels in the blood. In pregnancy, the kidneys already retain more fluid and electrolytes, so the margin for error narrows.
Possible maternal side effects:
- Headache, dizziness, or light‑headedness due to mild volume depletion.
- Elevated serum potassium, which can cause muscle weakness or cardiac arrhythmias.
- Gastrointestinal upset (nausea, diarrhea).
Fetal considerations:
- Excess maternal potassium can cross the placenta and affect fetal cardiac conduction.
- There is no clear evidence of structural birth defects, but the data pool is thin.
- Uncontrolled maternal hypertension itself poses greater risk to the fetus than the drug, making risk‑benefit assessment crucial.
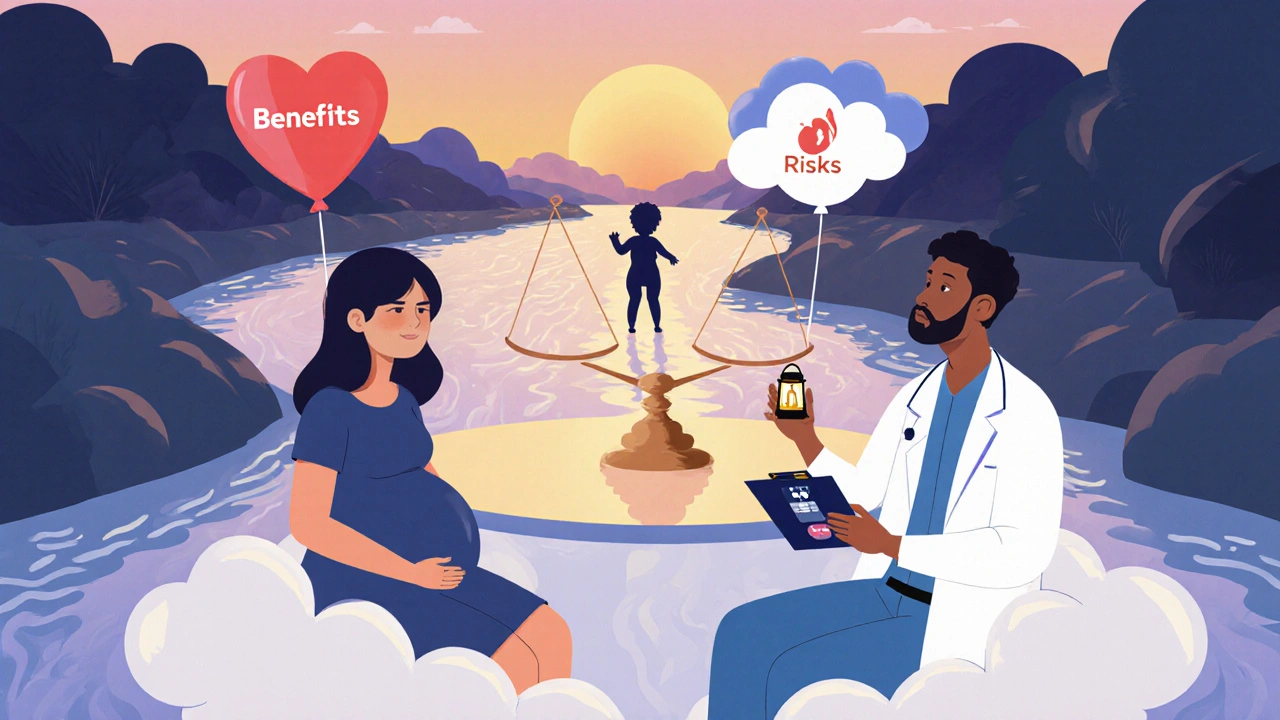
When Might a Doctor Choose Amiloride During Pregnancy?
Guidelines suggest reserving amiloride for cases where the benefit outweighs the uncertain risk. Typical scenarios include:
- Severe hypertension that does not respond to first‑line agents such as labetalol or nifedipine.
- Patients with chronic kidney disease where preserving potassium is essential and other diuretics could worsen electrolyte balance.
- Situations where spironolactone is contraindicated because of its anti‑androgen effects (e.g., in female fetuses with ambiguous genitalia risk).
In each case, the prescribing clinician should:
- Document the indication and discuss the uncertainty with the patient.
- Order baseline serum potassium and renal function tests.
- Monitor labs every 2-4 weeks throughout pregnancy.
- Consider dose reduction after the first trimester if blood pressure stabilizes.
Amiloride vs. Other Potassium‑Sparing Diuretics in Pregnancy
| Drug | Pregnancy Category (FDA) | Key Mechanism | Typical Indication | Special Considerations |
|---|---|---|---|---|
| Amiloride | C | ENaC blocker | Hypertension, CKD | Monitor K⁺, renal function; limited human data |
| Spironolactone | C | Aldosterone antagonist | Heart failure, ascites | Anti‑androgen effects; avoid if female fetus risk |
| Triamterene | C | ENaC blocker (similar to amiloride) | Adjunct to thiazides | Higher risk of crystal nephropathy; less studied |
All three fall into the same FDA category, but the choice often hinges on side‑effect profile and the patient’s underlying condition. Amiloride’s shorter half‑life and lower incidence of hormonal side effects give it a slight edge when potassium sparing is the main goal.
Breastfeeding Considerations
If you plan to breastfeed, the same caution applies. Amiloride does appear in breast milk in low concentrations, but data are insufficient to label it unsafe. The American Academy of Pediatrics lists it as “compatible with breastfeeding” provided infant serum potassium is monitored.
Practical steps:
- Check infant serum potassium if the mother has high levels.
- Observe the baby for signs of lethargy or feeding difficulties.
- Consider switching to an alternative antihypertensive if breast milk levels become a concern.
Key Takeaways Checklist
- Amiloride is Category C - limited human data, animal studies show some risk.
- Primary maternal concern is hyper‑kalemia; monitor labs regularly.
- Use only when hypertension or kidney disease cannot be managed with safer first‑line drugs.
- Compare with spironolactone and triamterene - amiloride often has fewer hormonal side effects.
- Breastfeeding is possible but requires infant potassium monitoring.
Frequently Asked Questions
Is amiloride safe in the first trimester?
The first trimester is the most sensitive period for drug exposure. Because amiloride is a Category C medication, it is generally avoided unless the mother’s hypertension is severe and cannot be controlled with other agents. If prescribed, the dose should be the lowest effective amount and labs monitored weekly.
What blood tests should be done while taking amiloride during pregnancy?
Baseline serum potassium, creatinine, and eGFR are essential. Repeat potassium and renal function every 2‑4 weeks, more often if doses are adjusted or if the patient develops edema or muscle weakness.
Can amiloride cause birth defects?
Current human data do not show a clear link to specific birth defects, but animal studies have reported growth retardation at high doses. The lack of robust evidence means clinicians weigh the known benefits for maternal health against the theoretical risk.
Should I stop amiloride after delivery?
Post‑partum blood pressure often rises, so many women continue a diuretic. However, if you plan to breastfeed, discuss with your doctor whether to keep amiloride or switch to another antihypertensive with a better lactation profile.
Are there lifestyle steps that reduce the need for amiloride in pregnancy?
Yes. Low‑salt diet, regular gentle exercise, and adequate hydration help manage blood pressure and fluid balance. These measures can often lower the required dose of any antihypertensive, including amiloride.
Bottom line: amiloride isn’t a first‑choice drug for most pregnant patients, but it can be a useful tool when hypertension or kidney disease demands a potassium‑sparing approach. The key is close monitoring, clear communication with your healthcare team, and a shared decision about risks versus benefits.



parth gajjar
October 19, 2025 AT 14:13The looming specter of medication during pregnancy turns each dose into a silent gamble that haunts every expectant mother a relentless chorus of doubt
Maridel Frey
October 21, 2025 AT 21:46Healthcare providers should approach amiloride therapy with clear communication and shared decision‑making. It is essential to explain the Category C classification in plain terms, emphasizing that the evidence is limited but the drug may be justified in severe hypertension. Regular monitoring of serum potassium and renal function should be scheduled every two to four weeks, and patients must understand the signs of hyperkalemia. Encouraging a low‑sodium diet and gentle exercise can also reduce reliance on pharmacologic intervention.
Jay Kay
October 24, 2025 AT 05:20Most of the time the article glosses over the real risk of potassium overload and pretends the data are reassuring. The truth is that without robust human trials we are guessing, and that guessing can cost a newborn its health.
Rakhi Kasana
October 26, 2025 AT 11:53While the caution you voice is valid, it is also important to recognize that uncontrolled maternal hypertension carries its own substantial fetal hazards. A nuanced assessment weighs both the potential for hyperkalemia and the dangers of persistent high blood pressure, rather than dismissing amiloride outright.
Sarah Unrath
October 28, 2025 AT 19:26its a risk but not a dealbreaker
James Dean
October 31, 2025 AT 03:00From a pharmacokinetic perspective the short half‑life of amiloride suggests that dose adjustments can be made relatively quickly should serum potassium trends rise. Nonetheless the physiological changes of pregnancy-expanded plasma volume and altered renal clearance-necessitate vigilant laboratory surveillance.
Monika Bozkurt
November 2, 2025 AT 10:33In the context of obstetric pharmacotherapy, amiloride occupies a niche characterized by its potassium‑sparing diuretic mechanism and its classification within the FDA Category C spectrum.
The mechanistic inhibition of the epithelial sodium channel (ENaC) curtails sodium reabsorption while preserving extracellular potassium stores.
Given the augmented intravascular volume and glomerular filtration rate observed in gestation, the renal excretion profile of amiloride may be modestly accelerated.
Conversely, the semi‑permeable nature of the placental barrier permits a transplacental flux of low‑molecular‑weight compounds, thereby introducing the potential for fetal exposure.
Empirical data from animal models have demonstrated dose‑dependent fetal growth retardation, albeit at supratherapeutic concentrations that exceed typical clinical dosing.
Human case series remain scarce, with the extant literature comprising fewer than a dozen documented pregnancies wherein amiloride was continued for refractory hypertension.
Within these reports, maternal serum potassium levels were maintained within normal limits through diligent biweekly monitoring, mitigating the theoretical risk of hyperkalemia.
Importantly, no teratogenic signal has been unequivocally attributed to amiloride, though the statistical power of existing studies is insufficient to exclude rare anomalies.
Clinical decision‑making should therefore integrate a risk‑benefit calculus that prioritizes the mitigation of severe maternal hypertension, a condition known to precipitate placental insufficiency and preeclampsia.
When alternative antihypertensives such as labetalol or nifedipine fail to achieve target blood pressures, amiloride may be considered as an adjunctive agent.
Baseline laboratory assessment ought to include serum potassium, creatinine, and estimated glomerular filtration rate, with subsequent assays scheduled at two‑ to four‑week intervals.
Dose titration is recommended to commence at the lowest effective regimen, with incremental adjustments contingent upon hemodynamic response and electrolyte stability.
In the postpartum period, the continuation of amiloride should be re‑evaluated in light of lactation considerations, acknowledging that trace amounts are detectable in breast milk.
If breastfeeding is pursued, infant serum potassium monitoring is advisable to preempt potential electrolyte disturbances.
Finally, a multidisciplinary approach involving obstetricians, nephrologists, and pharmacists can optimize therapeutic outcomes while safeguarding both maternal and fetal well‑being.
Through vigilant surveillance and collaborative care, amiloride can be deployed judiciously, transforming a theoretical concern into a manageable component of hypertensive management during pregnancy.
Penny Reeves
November 4, 2025 AT 18:06While the preceding exposition is exhaustive, it omits the practical nuance that many clinicians rely on real‑world pharmacovigilance databases rather than textbook pharmacodynamics. These registries often reveal that the incidence of clinically significant hyperkalemia in pregnant cohorts is under 1 % when protocols are adhered to. Consequently, the decision to prescribe amiloride should hinge less on theoretical teratogenicity and more on individualized risk profiling. In essence, the drug’s utility is defined by the clinician’s diligence, not by its categorical label.