When your hands feel clumsy, your balance starts to slip, or you keep dropping things you used to handle easily, it’s easy to blame aging. But if these changes are new, worsening, and paired with numbness in your arms or legs, it could be something more serious: cervical myelopathy. This isn’t just a stiff neck. It’s spinal cord damage caused by narrowing in your neck - a condition called cervical spinal stenosis. Left untreated, it can lead to permanent weakness, loss of coordination, or even paralysis. The good news? If caught early, surgery can stop the damage and even reverse some symptoms.
What Exactly Is Cervical Myelopathy?
Cervical myelopathy isn’t just stenosis - it’s what happens when that narrowing actually hurts your spinal cord. Think of it this way: spinal stenosis is the pipe getting smaller. Cervical myelopathy is when the water inside - your spinal cord - starts to drown. Most cases (about 75%) are caused by wear and tear over time, known as cervical spondylotic myelopathy (CSM). It’s not rare. Nearly 1 in 10 people over 70 have it, and it’s the most common cause of spinal cord problems in adults over 55. The spine in your neck normally has a canal about 17-18mm wide. When it shrinks to 13mm or less, it’s considered stenotic. At 10mm or under, the cord is under serious pressure. This happens because discs dry out and bulge, bones grow spurs, and ligaments thicken. These changes squeeze the spinal cord and the nerves running through it. The result? Signals from your brain to your hands and feet get scrambled.Early Warning Signs You Can’t Ignore
Many people dismiss early symptoms as carpal tunnel or just getting older. But there are specific red flags:- Hand clumsiness - struggling to button shirts, drop utensils, or turn keys
- Gait instability - feeling unsteady walking, especially in the dark or on uneven ground
- Numbness or tingling in hands, arms, or legs
- Increased reflexes - your doctor might notice your knee or ankle jerks harder than normal
- Balance problems - bumping into things, feeling like you’re walking on a boat
- Urinary urgency - needing to go more often, or not making it to the bathroom in time
How Doctors Diagnose It - It’s Not Just an X-Ray
A simple X-ray won’t cut it. You need an MRI. That’s the gold standard. It shows not just the narrowing, but whether the spinal cord itself is damaged - seen as bright spots on T2-weighted images. Without that signal change, you might just have stenosis without myelopathy. And yes, up to 21% of people over 40 have stenosis with no symptoms at all. Doctors use the Japanese Orthopaedic Association (JOA) score to measure severity. It checks motor function, sensation, and bladder control on a scale of 0 to 17. A score below 14 means you have myelopathy. A score below 12 usually means surgery is recommended. Other tests like CT myelography, EMG, or SSEPs help confirm nerve damage, especially if the MRI is unclear. But the diagnosis always needs both symptoms and imaging. You can’t just rely on pain. Only about half of people with cervical myelopathy even have neck pain.When Is Surgery the Only Real Option?
Conservative treatment - physical therapy, NSAIDs, activity changes - might help if your symptoms are mild and stable. But here’s the hard truth: 63% of people with mild myelopathy get worse over two years without surgery. Only 28% improve. If your JOA score is below 12, or if symptoms are getting worse, surgery isn’t just an option - it’s the standard of care. The American Academy of Orthopaedic Surgeons gives this a strong Grade A recommendation. Why? Because the spinal cord doesn’t heal well once damaged. The longer you wait, the less you can recover. Studies show that patients who have surgery within six months of symptoms starting recover 37% better than those who wait over a year. Recovery drops by about 3% for every month you delay. That’s not a small window.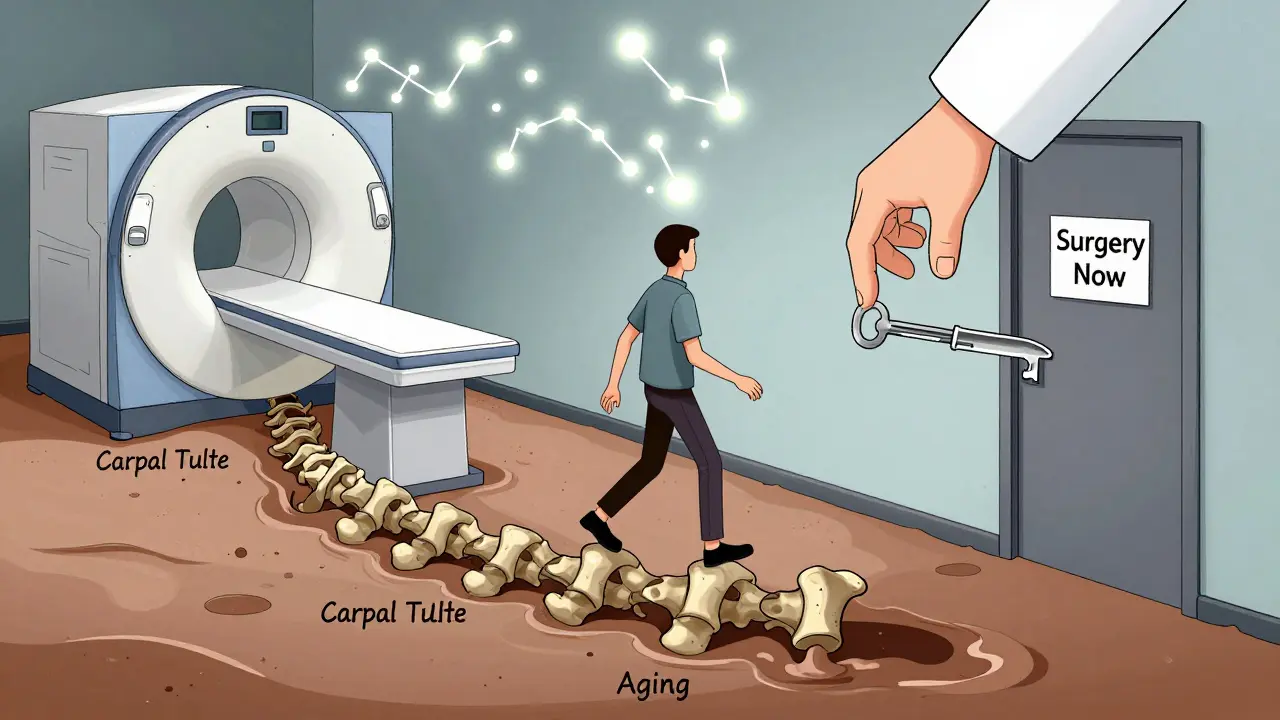
Types of Surgery - Anterior vs. Posterior
There are three main approaches:- Anterior Cervical Discectomy and Fusion (ACDF): The surgeon goes in from the front, removes the damaged disc and bone spurs, and fuses the vertebrae. Best for single or two-level problems. Success rate? Around 85-90% for neurological improvement. But 5-7% of patients develop new problems in nearby discs within 10 years.
- Cervical Disc Arthroplasty: Similar to ACDF, but instead of fusing, they replace the disc with an artificial one. Approved for multi-level use since 2023. Preserves motion, reduces future fusion risks. Early results show 81% success at two years.
- Posterior Approaches: Laminectomy (removing the back part of the bone), laminoplasty (hinging the bone open), or laminectomy with fusion. Used for multi-level stenosis or when the spine is unstable. Laminoplasty has less post-op neck pain (15% vs. 32%) but slightly lower neurological recovery (78% vs. 85%).
What to Expect After Surgery
Hospital stays are short: 1-2 days for anterior, 2-3 for posterior. Recovery takes 3-6 months. You’ll need formal physical therapy for 8-12 weeks. Focus? Cervical stability, gait retraining, and regaining hand coordination. Most people (82%) report better hand function after surgery. But only 65% regain normal walking ability. About 28% still need a cane or walker. That’s not failure - it’s realistic. The goal isn’t always to go back to how you were at 40. It’s to stop the decline and get back to what matters: dressing yourself, walking without fear, controlling your bladder.Common Problems After Surgery
No surgery is risk-free. About 4-6% of patients face major complications:- C5 nerve palsy - weakness in the shoulder or upper arm (happens in 5-10% of cases)
- Dysphagia - trouble swallowing (22% in first 3 months after anterior surgery)
- Chronic neck pain - especially after posterior surgery (18% develop "post-laminectomy syndrome")
- Neurological worsening - rare, but 1-2% of patients end up worse





John Rose
January 29, 2026 AT 09:23Just had my MRI last week after dropping my coffee mug 5 times in 10 minutes. Turned out I had CSM at L13mm. Doctor said if I’d waited another 6 months, I might’ve needed a cane permanently. Got ACDF last month - fingers are already less clumsy. Don’t ignore the small stuff. It’s not aging, it’s your spine screaming.
Mark Alan
January 29, 2026 AT 12:49THIS IS WHY AMERICA IS FALLING APART 😭 People are too lazy to move, eat junk, and then blame their spine for being weak. I’ve been doing 100 push-ups a day since I was 12. My neck’s stronger than your entire office chair. If you’re dropping things, maybe stop scrolling TikTok and lift something real. 🤬
Amber Daugs
January 29, 2026 AT 23:56Wow. So you’re telling me people are just letting their bodies rot until they need surgery? No wonder the healthcare system is broken. I’ve been doing yoga every morning since 2015. My spine is a cathedral. If you’re reading this and you’re over 50 and still sitting at a desk 10 hours a day - you’re not a victim, you’re negligent. 🙄
Ambrose Curtis
January 30, 2026 AT 06:49Man, I read this whole thing and I’m glad I didn’t wait. My doc said I had mild CSM last year - JOA score was 13. I did PT for 6 months, but when my grip kept fading, I got the MRI. Saw the bright spot on T2 like a neon sign. Got laminoplasty. Took 4 months to feel normal again, but now I can hold a fork without my hand shaking. If you’re reading this and you’ve been saying ‘oh it’s just arthritis’ - stop. Go get an MRI. Don’t be like me and wait till you drop your grandkid’s bottle.
Also, riluzole sounds wild. I heard they’re testing it in Boston. If it helps even 10%, it’s a game changer. Don’t let fear stop you. Surgery isn’t the end - it’s the reset button.
Robert Cardoso
January 31, 2026 AT 08:42Let’s be honest - this entire narrative is manufactured by orthopedic conglomerates. The data cherry-picks patients who were already declining. The 63% deterioration statistic ignores spontaneous stabilization. And let’s not forget that 21% of people over 40 have stenosis with zero symptoms - meaning MRI findings ≠ pathology. You’re pathologizing aging. Cervical myelopathy is real, but the surgical industrial complex is profiting off fear, not science.
Also, the JOA scale? Developed in 1975. It doesn’t account for cognitive load, fatigue, or comorbidities. And you call that ‘gold standard’? Please. The real issue is that primary care physicians lack training in neurologic screening. Blame the system, not the patient.
Katie Mccreary
January 31, 2026 AT 15:11So you’re telling me I should get surgery because I can’t button my shirt? I’m 58. I’ve been dropping things since I was 40. Maybe I just have small hands. Or maybe I’m tired. Or maybe I’m not a robot who needs to be ‘fixed.’
SRI GUNTORO
February 1, 2026 AT 06:28In India, we don’t rush to surgery. We use Ayurveda, massage, and patience. Your body heals when you listen to it - not when you cut it open. Why do you trust machines more than your own spirit?
Kevin Kennett
February 1, 2026 AT 18:54Hey, I just want to say - if you’re reading this and you’re scared, you’re not alone. I was terrified of surgery too. But my mom had this done last year. She went from barely walking to gardening again. It’s not magic. It’s medicine. And yeah, recovery sucks. But so does living in fear. You don’t have to be ‘fixed’ to be whole. Just don’t wait. Talk to someone who’s been there. I’ll send you my therapist’s number if you need it.
Howard Esakov
February 3, 2026 AT 16:41Of course you need surgery. Anyone who doesn’t act immediately after noticing neurological symptoms is either delusional or willfully ignorant. I read the JAMA paper. The data is irrefutable. You’re not ‘getting older’ - you’re losing motor neurons. And if you think yoga or ‘energy healing’ will fix a compressed spinal cord, you’re not just wrong - you’re endangering others by spreading misinformation.
Rhiannon Bosse
February 3, 2026 AT 17:20Wait… so you’re telling me the government is letting Big Spine profit off our fear? And they’re using MRI scans to scare us into surgery? I knew it. They’re injecting nanobots through the spinal canal to track us. That’s why they say ‘don’t delay’ - it’s not about healing, it’s about control. 😈👁️🗨️
Bryan Fracchia
February 4, 2026 AT 11:51There’s a quiet truth here: we’re all going to break down eventually. The spine, the knees, the heart - they’re not designed to last 80 years on processed food and Zoom calls. But what’s beautiful is that we still have the power to intervene. Surgery isn’t surrender. It’s an act of care. Not because we’re broken, but because we still want to hold our grandkids, tie our shoes, and feel the wind without fear. That’s not weakness. That’s humanity.