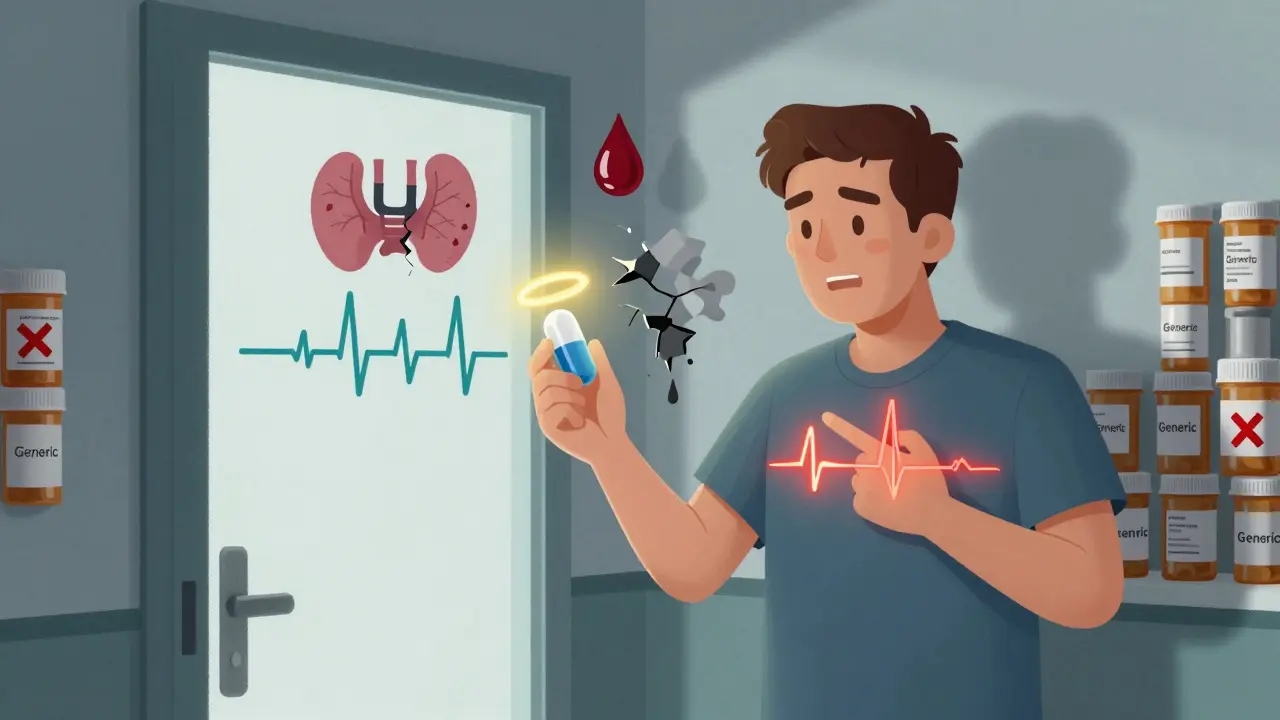
Switching from a brand-name medication to a generic version sounds simple - cheaper, same active ingredient, right? But for many people, that switch doesn’t go smoothly. Some notice changes in how they feel - more side effects, less control over their condition, or even a return of symptoms they thought were under control. If you’ve been on a brand-name drug for years and your pharmacy suddenly gives you a different pill, you’re not alone. And you have every right to speak up.
Why Some People Can’t Switch to Generics
Not all generics are created equal, even if they contain the same active ingredient. The FDA says generics must be bioequivalent to the brand - meaning they deliver the same amount of medicine into your bloodstream at the same rate. But there’s a catch: the allowed range for bioequivalence is 80% to 125% of the brand’s performance. For most drugs, that’s fine. For others - especially those with a narrow therapeutic index - even small differences matter. Drugs like warfarin (for blood thinning), levothyroxine (for thyroid), and anti-seizure medications like phenytoin or levetiracetam fall into this category. Studies show a 23% higher chance of seizure recurrence when switching from brand-name Keppra to a generic version. With warfarin, switching between generic manufacturers led to a 17% increase in emergency room visits because blood levels became unstable. These aren’t rare cases. Around 14% of doctors report seeing patients who clearly respond differently to generics. Another issue? Inactive ingredients. Generics use different fillers, dyes, or preservatives. If you’re allergic to lactose, gluten, or certain food dyes - and your brand drug doesn’t contain them - switching could trigger a reaction. About 7% of patients report allergic or gastrointestinal issues linked to these additives in generics. If you’ve ever felt bloated, itchy, or dizzy after a pill change, it might not be in your head.What to Do Before Your Appointment
Don’t walk into your doctor’s office hoping they’ll just listen. Show up prepared. Bring proof. A vague complaint like “I don’t like the generic” won’t cut it. But a clear record of what happened will. Start by keeping a simple journal. Write down:- The date you switched to the generic
- What symptoms changed - fatigue, headaches, mood swings, seizures, etc.
- How bad they were on a scale of 1 to 10
- When they improved after switching back to the brand
How to Talk to Your Doctor
Use a simple structure that works: Situation, Background, Assessment, Recommendation - or SBAR. It’s used by nurses and doctors for a reason: it gets results. Here’s how it sounds:- Situation: “I’ve been on brand-name Keppra for five years. My seizures were under control.”
- Background: “When my pharmacy switched me to the generic last November, I had three seizures in two months. I went back to the brand, and they stopped.” Assessment: “I believe the generic isn’t working for me. My lab results show my blood levels dropped after the switch.”
- Recommendation: “Can we keep me on the brand? I’d like you to write ‘Dispense as Written’ on the prescription.”

Insurance and Prior Authorization
Here’s where it gets tricky. Most insurance plans push generics because they’re cheaper. In fact, 82% of commercial health plans in the U.S. require you to try the generic first. If you want the brand, your doctor has to jump through hoops. They’ll need to submit a prior authorization request. That’s paperwork. And it’s not easy. About 43% of doctors say they spend 15 to 30 minutes per patient filling out these forms. Some even prescribe generics they don’t think are right for you - just to avoid the delay. Your job? Make it easy for them. Give them everything they need:- Your symptom journal
- Lab results showing instability
- Proof of allergic reaction (if applicable)
- A copy of your pharmacy’s substitution history
What If Your Doctor Says No?
Sometimes, doctors still say no. Maybe they think the generic is fine. Maybe they’re pressed for time. If that happens, don’t argue. Ask for a second opinion. You can request a referral to a specialist - like a neurologist for epilepsy, an endocrinologist for thyroid meds, or a hematologist for blood thinners. Specialists are more likely to recognize when a brand is medically necessary. They also have more experience navigating insurance appeals. You can also contact your insurance company directly. Most have a patient advocate or appeals department. Ask them what documentation they need to approve the brand. Then give that to your doctor. It’s not about fighting - it’s about working together.
What About the Cost?
Yes, brand-name drugs cost more. But here’s the reality: generics make up 90% of prescriptions but only 15% of drug spending. Brand drugs cost way more - and that’s why insurers push them. If you’re on Medicare Part D, you can request a coverage exception. About 57% of those requests are approved when you have clinical proof. Some drug manufacturers offer patient assistance programs. Check the brand’s website - many have coupons or free trials for people who qualify. Don’t assume you can’t afford it. Ask.Final Thoughts
You know your body better than anyone. If something changed after a switch - and it’s affecting your health - speak up. You’re not being difficult. You’re being smart. The system isn’t perfect. Generics save money. But for some people, they don’t work. And that’s okay. Your health isn’t a cost-cutting experiment. Document your experience. Bring facts to your appointment. Use clear language. And remember - you have the right to ask for what works for you.Can my pharmacist switch my brand medication without telling me?
In most states, yes - unless your doctor writes "Dispense as Written" (DAW-1) on the prescription. Forty-seven states allow pharmacists to substitute generics without patient consent. Twelve states require the patient to agree first. Always check your prescription label and ask if your pill looks different.
Are generics less effective than brand-name drugs?
For most drugs, yes - they’re just as effective. But for medications with a narrow therapeutic index - like warfarin, levothyroxine, and anti-seizure drugs - small differences in absorption can lead to real health risks. Studies show higher rates of hospital visits and symptom return when switching these types of drugs to generics.
What if I can’t afford the brand medication?
Talk to your doctor. Many brand-name manufacturers offer patient assistance programs, coupons, or free samples. Medicare Part D has a coverage exception process. You can also ask about alternative brands or dosing strategies - sometimes splitting a higher-dose pill can save money. Never stop taking your medication because of cost. There are always options.
Can I ask for a specific generic manufacturer?
Yes - but it’s not guaranteed. Some pharmacies carry generics from different manufacturers, and one might work better for you than another. Ask your pharmacist if they have multiple versions. If one makes you feel worse, request a different one. Some doctors will write "Do Not Substitute" or specify a manufacturer on the prescription.
Is it true that generics are made in the same factories as brand drugs?
Sometimes. Many brand-name companies also make generic versions of their own drugs. The FDA inspects both types of facilities to the same standards. But the inactive ingredients - the fillers, dyes, and binders - often differ. That’s why some people react differently, even if the active ingredient is identical.




Mike Hammer
February 13, 2026 AT 20:36Man, I switched my levothyroxine last year and suddenly I was a zombie. No energy, brain fog, cold all the time. Thought I was going insane. Turned out the generic had a different filler-lactose. I’m lactose intolerant. My pharmacist didn’t even blink when they handed me the new pill. Now I always check the label. If it looks different, I ask. No shame in that.
Sarah Barrett
February 14, 2026 AT 21:49There’s a quiet revolution happening in pharmacology-one that doesn’t make headlines but saves lives. The assumption that generics are interchangeable is a myth dressed in bureaucratic clothing. For those of us navigating chronic conditions, the difference between a pill that works and one that destabilizes isn’t theoretical-it’s measured in heartbeats, seizures, and sleepless nights. We’re not asking for luxury; we’re demanding biological fidelity.
The FDA’s 80–125% bioequivalence window is a statistical loophole, not a clinical guarantee. When your thyroid hormone dips below the threshold because of a change in coating, you don’t get a memo. You just feel like you’re fading. And yes, the inactive ingredients? They’re not inert. They’re chemical signatures. A dye, a binder, a preservative-they can trigger reactions in sensitive bodies. This isn’t placebo. It’s pharmacology with its eyes closed.
Bringing lab results, symptom logs, and even the physical pills to your appointment? That’s not being difficult. That’s being a scientist of your own body. And doctors who dismiss this? They’re not being pragmatic-they’re being negligent. The system rewards volume, not vigilance. But we’re changing that-one documented case at a time.
Daniel Dover
February 16, 2026 AT 09:35DAW-1 code. Always ask for it. Simple.
Mandeep Singh
February 17, 2026 AT 21:33Oh please. Another ‘I’m special because my body doesn’t work like everyone else’s’ sob story? Let me guess-you’re also allergic to sunlight and think your Wi-Fi signal is plotting against you? The FDA doesn’t approve generics based on mood swings or ‘vibes.’ They use science. Real science. Blood levels. Pharmacokinetics. Peer-reviewed studies. Not your ‘I felt weird after switching’ diary.
And let’s not forget: 90% of prescriptions are generics for a reason. Because they work. For 99% of people. You’re the outlier. The exception. The 1%. Stop demanding special treatment because you can’t tolerate a slightly different starch filler. Get over it. Or better yet-see a specialist who actually knows what they’re doing instead of whining to your GP about pill color.
And don’t even get me started on the ‘brand-name is better’ myth. If you’re paying $500 a month for a drug that’s available as a $5 generic, you’re not being smart-you’re being exploited by Big Pharma’s marketing machine. Wake up.
Josiah Demara
February 18, 2026 AT 09:36Let’s cut through the emotional noise. The data doesn’t lie. A 23% increase in seizure recurrence with generic levetiracetam? That’s not anecdotal-it’s published in NEJM. A 17% spike in ER visits for warfarin switches? That’s in Circulation. This isn’t about ‘feeling different.’ It’s about measurable, reproducible, statistically significant clinical outcomes.
People who say ‘it’s all in your head’ haven’t read the literature. They’ve read Reddit threads. The FDA’s bioequivalence standard is a regulatory convenience, not a medical truth. Narrow therapeutic index drugs? They’re not ‘special cases.’ They’re the rule for critical medications. If you’re prescribing levothyroxine, warfarin, or anticonvulsants without considering manufacturer variation-you’re not a doctor. You’re a gambler.
And the insurance push for generics? It’s not cost-saving. It’s cost-shifting. You save $20 on the drug, then spend $8,000 on an ER visit because the patient had a stroke from unstable INR. That’s not fiscal responsibility. That’s negligence dressed as efficiency.
Document everything. Demand DAW-1. Appeal denials. This isn’t advocacy-it’s survival. And if your doctor won’t fight for you? Find one who will. Your life isn’t a spreadsheet.
Kaye Alcaraz
February 19, 2026 AT 01:50You’ve got this. You’re not asking for something unreasonable. You’re asking for your body to be respected. That’s not too much to ask. Keep that journal. Print those lab results. Bring the pills. Be calm. Be clear. Be persistent. Doctors are humans too. They want to help. Give them the tools. And if they say no? Keep going. One appeal at a time. You’re not alone.
Erica Banatao Darilag
February 20, 2026 AT 11:21I switched to a generic for my seizure med and had two seizures in three weeks. My doctor said it was ‘probably stress.’ I brought my log, my INR levels, and the actual pills. He looked at them. Said ‘I didn’t know that happened.’ Wrote DAW-1 that day. I’m not a drama queen. I’m just someone who lived through it. If you’re feeling off after a switch? You’re not crazy. You’re just paying attention.
Charlotte Dacre
February 21, 2026 AT 09:49So let me get this straight. We’ve got a system where your life depends on the color of a pill, but the only way to fix it is to become a medical detective, submit a 17-page dossier, and beg your doctor to do paperwork for you? Oh, and if you’re lucky, maybe you’ll get the brand-after your insurance denies it twice and your pharmacist sighs like you asked for a unicorn.
How about we just… stop pretending this is healthcare and call it what it is: a bureaucratic obstacle course with a side of placebo effect and a sprinkle of corporate greed? I mean, at least the FDA lets us know which generics are ‘equivalent.’ But good luck finding that list. It’s buried under 12 layers of PDFs and a paywall. Welcome to medicine, folks. Where your health is a cost center and your voice? A footnote.