What Are Topical Antihistamine Eye Drops?
Topical antihistamine eye drops are designed to treat allergic conjunctivitis - that itchy, red, watery eye condition you get when pollen, dust, or pet dander triggers your immune system. Unlike oral antihistamines that make you sleepy or dry out your mouth, these drops work right where the problem is: your eyes. They block histamine, the chemical your body releases during an allergic reaction, before it can cause swelling and itching.
Common brands include Ketotifen (a dual-action antihistamine and mast cell stabilizer available over-the-counter as Alaway or Zaditor), Olopatadine (a prescription option like Pataday that lasts up to 24 hours), and Azelastine (sold as Optivar, works fast but can taste bitter). These aren’t just quick fixes - they’re the first-line treatment recommended by the American Academy of Ophthalmology for allergic eye symptoms.
How Quickly Do They Work?
One of the biggest advantages of these drops is speed. Most people feel relief within 3 to 15 minutes after applying them. In clinical trials, olopatadine 0.7% reduced itching by over 80% within just 3 minutes. That’s faster than most oral allergy pills. If you’re stuck in a room full of cat hair or walking through a pollen-heavy park, these drops can turn a miserable experience into something manageable.
But duration varies. Ketotifen (Alaway) usually lasts about 8 to 12 hours, so you’ll need to use it twice a day. Olopatadine 0.7% (Pataday) is formulated to last a full 24 hours, meaning one drop in the morning is often enough. That’s why many people switch to olopatadine if they’re using ketotifen daily - fewer applications, better compliance.
Common Side Effects
Most people tolerate these drops well, but they’re not side effect-free. The most common complaint? A brief stinging or burning sensation right after putting them in. About 41% of first-time users report this, according to a 2022 study in Clinical Ophthalmology. It lasts less than a minute. Cooling the bottle in the fridge before use helps reduce this feeling.
Other side effects include:
- Headache (reported in 12% of users)
- Dry eyes (especially with long-term use)
- Blurred vision (temporary, clears within seconds)
- Unpleasant taste in the mouth (common with azelastine - about 18% of users notice it due to drainage through the tear duct into the throat)
Preservatives like benzalkonium chloride (BAK), found in multi-dose bottles, can irritate sensitive eyes. If you’re using drops every day for weeks, you might notice increased redness or discomfort. That’s why some brands now offer preservative-free, single-use vials - like Lastacaft (olopatadine 0.2%) - to reduce this risk.
When Not to Use Them
These drops only work for allergic eye conditions. If your eyes are red, painful, and producing thick yellow or green discharge, you likely have bacterial conjunctivitis - not allergies. Using antihistamine drops here won’t help. In fact, delaying proper treatment can lead to corneal damage.
They also won’t fix dry eye syndrome unless it’s caused by allergies. If your eyes feel gritty, tired, or sore all day - even when pollen counts are low - you might need lubricating drops or other treatments. Misdiagnosing dry eye as allergies is one of the most common mistakes people make.
And if you’ve been using them for more than 12 weeks without seeing a doctor, stop. Long-term use can mask underlying problems like glaucoma or chronic inflammation. The FDA has documented cases where prolonged use led to unnoticed increases in eye pressure, especially in people already at risk.
Proper Use: How to Apply Them Right
Getting the most out of these drops means using them correctly. Here’s how:
- Wash your hands before handling the bottle.
- Don’t let the dropper tip touch your eye, eyelid, or any surface. Contamination can cause infections.
- Tilt your head back, pull down your lower eyelid to form a pocket, and drop one drop into that pocket.
- Close your eye gently for 30 seconds. Press lightly on the inner corner of your eye (near the nose) to prevent the drop from draining into your throat.
- If you’re using more than one type of eye drop, wait at least 5 to 10 minutes between each. Otherwise, the second drop will just wash out the first.
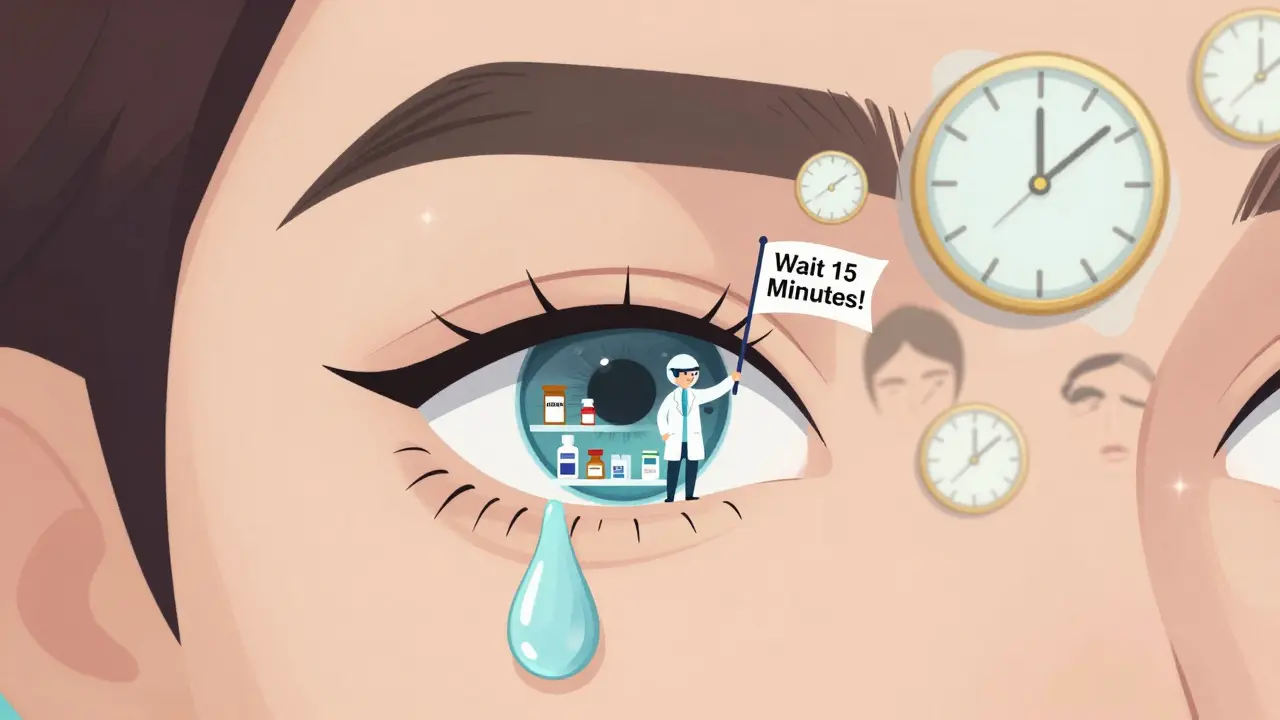
- If you wear contact lenses, remove them before applying the drops. Wait at least 10 to 15 minutes after using them before putting lenses back in.
Many people skip the last step - and end up with irritation or even infections. A 2023 FDA report found 147 cases of contact lens-related complications directly linked to reinserting lenses too soon after using eye drops.
OTC vs. Prescription: Which One Should You Choose?
There’s a big difference between what you can buy at the pharmacy and what your doctor prescribes.
| Brand | Active Ingredient | Strength | Dosing | Price (USD) | Best For |
|---|---|---|---|---|---|
| Alaway, Zaditor | Ketotifen | 0.025% | Twice daily | $15-$25 (OTC) | Intermittent use, budget-friendly |
| Pataday | Olopatadine | 0.7% | Once daily | $85-$120 (Rx) | Daily allergy sufferers, long-lasting relief |
| Optivar | Azelastine | 0.05% | Twice daily | $70-$100 (Rx) | Faster relief, but bitter taste |
OTC options like ketotifen are great for occasional symptoms - say, during spring pollen season. But if you’re using them every day for months, it’s worth talking to your doctor. Prescription olopatadine offers better control, fewer doses, and often fewer side effects over time.
When to See a Doctor
You don’t need to see a doctor for every case of itchy eyes. But here’s when you should:
- Your eyes are still red or swollen after 72 hours of using the drops
- You notice vision changes, light sensitivity, or eye pain
- Your symptoms get worse instead of better
- You’ve been using OTC drops for more than 16 weeks
- You wear contact lenses and develop persistent irritation
The FDA requires all OTC eye drop labels to say: “Stop use and ask a doctor if symptoms last more than 72 hours.” That’s not just a legal footnote - it’s a warning based on real cases. In 2018, 127 people ended up with chemical conjunctivitis because they kept using antihistamine drops for bacterial or viral infections.

Real User Experiences
People on Reddit and Drugs.com talk about ketotifen like it’s a miracle - until they hit the stinging phase. One user wrote: “Zaditor gives me 12 hours of relief, but the first minute feels like I dropped hot sauce in my eye.” That’s normal. Most users say the burn fades fast.
Others who switched from ketotifen to olopatadine report fewer issues overall. “I used Alaway for two years,” said a 38-year-old teacher from Ohio. “Then I tried Pataday once daily. No more stinging, no more twice-daily reminders. My eyes feel better than they have in years.”
But there are warning stories too. One woman in Texas used ketotifen daily for 6 months to treat “dry eyes.” Turns out, she had early-stage glaucoma. The drops masked the inflammation, and her eye pressure kept climbing. By the time she saw a specialist, she’d lost 15% of her peripheral vision.
What’s New in 2026?
The field is evolving. In 2023, the FDA approved a new nanoemulsion version of olopatadine (Lastacaft) that reduces preservative irritation. That’s a big win for people who used to stop using drops because their eyes got too dry.
Researchers are also testing combinations - like ketotifen with low-dose steroids - for severe allergies like vernal keratoconjunctivitis, especially in kids. Results are expected in mid-2024.
But there’s a growing concern: overuse. With 62% of people self-treating before seeing a doctor, misdiagnosis is rising. The CDC reported a 12% jump in antibiotic-resistant bacterial strains linked to people using antihistamine drops for infections. That’s why eye doctors now push harder for proper diagnosis before recommending any treatment.
Final Thoughts
Topical antihistamine eye drops are safe, effective, and fast - if used the right way. They’re not a cure-all, and they’re not meant for long-term, unsupervised use. If you have seasonal allergies, they can be a game-changer. But if your symptoms don’t improve in a few days, or if you’re relying on them daily for months, it’s time to get checked out.
Keep your eyes healthy: know what you’re using, follow the instructions, and don’t ignore warning signs. Your vision is worth more than a bottle of drops.
Can I use antihistamine eye drops with contact lenses?
Yes, but you must remove your lenses before applying the drops. Wait at least 10 to 15 minutes after using them before putting your contacts back in. Reinserting lenses too soon can trap the medication and preservatives against your eye, increasing the risk of irritation or infection. Some brands offer preservative-free versions specifically for contact lens wearers - ask your doctor.
Do antihistamine eye drops make you sleepy?
No, not usually. Unlike oral antihistamines like Benadryl, topical eye drops are designed to stay localized in the eye. Very little enters your bloodstream, so drowsiness is rare. However, if you accidentally swallow a large amount - say, by not pressing your tear duct after application - you might feel slightly drowsy. That’s why it’s important to press the inner corner of your eye for 30 seconds after each drop.
How long do antihistamine eye drops last once opened?
Multi-dose bottles typically last 28 days after opening, even if they’re not empty. After that, the risk of bacterial contamination increases. Single-use vials are discarded after one use. Always check the expiration date on the bottle and follow the manufacturer’s instructions. Never use drops past their expiration date or if they look cloudy or discolored.
Are antihistamine eye drops safe for children?
Yes, certain formulations are approved for children as young as 3 years old. Ketotifen (Children’s Alaway) is commonly used in kids with seasonal allergies. Always check the label for age recommendations and use the correct dosage. If your child has persistent eye symptoms, see a pediatric ophthalmologist - allergies can sometimes mimic other conditions like conjunctivitis or eyelid inflammation.
Can I use antihistamine eye drops with other eye medications?
You can, but timing matters. Always wait at least 5 to 10 minutes between different eye drops. Use antihistamine drops first, followed by lubricating drops or other treatments. This ensures the antihistamine stays in contact with the eye long enough to work. Never mix different drops in the same bottle - it can cause chemical reactions or reduce effectiveness.





Juan Reibelo
January 23, 2026 AT 14:08Also, never skip pressing the inner corner of your eye. I learned that the hard way after accidentally swallowing a drop and feeling like I'd been drugged by a sleepy bee.
Josh McEvoy
January 23, 2026 AT 21:57Heather McCubbin
January 25, 2026 AT 01:12Himanshu Singh
January 25, 2026 AT 21:05Jamie Hooper
January 27, 2026 AT 02:49Husain Atther
January 27, 2026 AT 03:21Izzy Hadala
January 27, 2026 AT 16:17Elizabeth Cannon
January 29, 2026 AT 16:09Phil Maxwell
January 30, 2026 AT 13:00Tommy Sandri
January 31, 2026 AT 00:10