Myeloma Radiation Therapy Dose Calculator
Treatment Settings
Estimated Treatment Plan
Potential Side Effects
- Skin irritation
- Fatigue
Blood Count Monitoring
Your care team will monitor blood counts before, during, and after treatment.
When you hear “radiation therapy” in a myeloma conversation, it can feel like a foreign language. Radiation therapy is a localized treatment that uses high‑energy photons or particles to destroy cancer cells in a specific area. Multiple myeloma is a blood‑cancer that primarily grows in the bone marrow, causing bone pain, fractures, and abnormal blood counts. Understanding how myeloma radiation therapy fits into the overall care plan helps you ask the right questions and feel more in control of your journey.
Why Radiation Therapy Is Used in Myeloma
Radiation isn’t a cure for myeloma, but it shines when the disease creates a single problem spot. Typical reasons include:
- Relieving painful bone lesions that haven’t responded to systemic drugs.
- Stabilizing a fracture or preventing an impending break.
- Preparing a bone for a surgical procedure.
- Controlling a solitary plasmacytoma (a localized collection of myeloma cells).
In these cases the goal is usually palliative - to improve quality of life - rather than to eradicate the disease everywhere in the body.
How the Treatment Is Planned
The first step is a simulation appointment. A CT scan creates a three‑dimensional map of the targeted area, allowing the radiation oncologist to define the exact shape of the tumor. An MRI may be added if soft‑tissue detail is essential. The radiation team then designs a treatment plan using specialized software that calculates the optimal beam angles, energy levels, and doses - a process called dosimetry.
During planning, a radiation oncologist reviews the images, discusses goals with you, and decides whether you need a curative‑intent dose (higher, longer) or a palliative dose (lower, shorter).
Types of Radiation Used for Myeloma
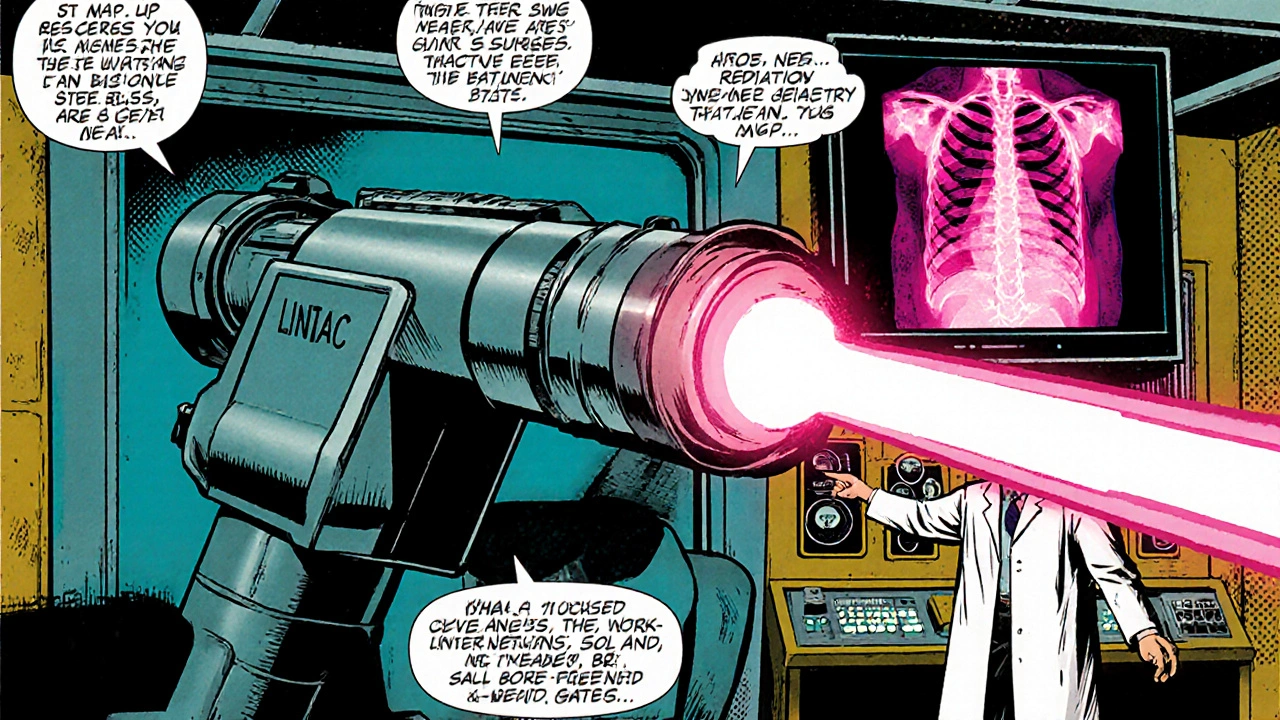
Most myeloma patients receive external beam radiation therapy (EBRT). It delivers photons from a machine called a linear accelerator (LINAC) that sits outside your body. For very small, well‑defined lesions, stereotactic body radiation therapy (SBRT) can give a higher dose in fewer sessions, shrinking treatment time from weeks to a handful of visits.
In rare cases, a bone‑seeking radioisotope such as radium‑223 may be prescribed. This is a systemic form of radiation that travels to bone lesions throughout the skeleton, but it’s considered a separate line of therapy rather than local radiation.
Typical Radiation Schedules
For painless, stable lesions, doctors often use a short course: 8 Gy in a single session or 20 Gy over five daily fractions. If the goal is more aggressive pain control, a slightly longer regimen like 30 Gy in ten fractions is common. Your schedule will depend on the size of the target, its location, and how well your overall health tolerates radiation.
Side Effects You Might Experience
Because radiation is focused, side effects are usually limited to the treatment field. Common issues include:
- Skin irritation: Redness, itching, or a mild sunburn‑like feeling that usually resolves a few weeks after treatment.
- Fatigue: A gradual tiredness that can build up over the week of treatment.
- Localized pain flare: Some patients feel a temporary increase in pain a few days after the first fraction.
- Bone marrow suppression: If a large portion of marrow is in the field, blood counts may dip, requiring closer monitoring.
Serious complications-like fractures of irradiated bones or radiation‑induced secondary cancers-are rare but worth discussing, especially if you’re younger or expect many future treatments.
Managing Side Effects and Staying Comfortable
Here are practical tips you can start using right away:
- Keep the treated skin clean and dry. Use mild soap and avoid harsh chemicals.
- Apply a fragrance‑free moisturizer after the skin cools down (usually a few hours post‑session).
- Stay hydrated; water helps skin recover and reduces fatigue.
- Ask your team about topical steroids or pain‑relief gels if skin irritation becomes bothersome.
- Schedule light activity-short walks, gentle stretching-to combat fatigue without overexertion.
- Report any unexpected swelling, numbness, or worsening pain to your radiation oncologist immediately.
Most side effects improve within 2-4 weeks after completing treatment, but keep your follow‑up appointments so the team can verify that the lesion is responding as expected.
Radiation vs. Other Myeloma Treatments
| Aspect | Radiation Therapy | Systemic Therapy (e.g., chemotherapy, immunotherapy) |
|---|---|---|
| Target Scope | Localised to a specific bone or lesion | Whole‑body; reaches all bone marrow sites |
| Primary Goal | Pain relief, fracture prevention, local control | Disease‑wide control, remission, prolong survival |
| Typical Duration | 1‑3 weeks (depending on fractionation) | Weeks to months, often continuous cycles |
| Side‑Effect Profile | Localized skin, fatigue, possible marrow suppression | Systemic nausea, infection risk, neuropathy |
| When Used | Isolated painful lesions, pre‑surgical preparation | Throughout disease course, especially early‑stage |
The table shows that radiation is a complementary tool rather than a replacement for chemotherapy, stem‑cell transplant, or newer agents like proteasome inhibitors.
Key Takeaways
- Radiation is most effective for single, painful bone lesions or to prevent fractures.
- A short simulation (CT/MRI) maps the target, and a radiation oncologist designs the dose.
- Side effects are usually mild and limited to the treatment area, but monitoring blood counts is essential.
- Radiation works alongside systemic therapies-talk to your team about how it fits your overall plan.
- Stay proactive: moisturize skin, stay hydrated, and report any new symptoms promptly.
Frequently Asked Questions
Is radiation therapy curative for myeloma?
No. Myeloma is a systemic disease, so radiation can’t cure it. The treatment is used to control specific problems, such as painful bone lesions, and to improve quality of life.
How many treatment sessions will I need?
It depends on the goal. A single‑session “8Gy” plan may be enough for mild pain, while a broader palliative course often uses 10‑20 sessions spread over two weeks.
Will radiation affect my blood counts?
If the radiation field includes a large amount of active marrow, you may see a temporary dip in white cells or platelets. Your oncologist will order blood tests before, during, and after treatment to catch any issues early.
Can I combine radiation with chemotherapy?
Yes, many patients receive both. Timing is coordinated so that chemotherapy doesn’t increase skin toxicity. Your care team will schedule the two modalities to minimize overlap.
What should I bring to my simulation appointment?
Wear comfortable clothing without metal zippers, bring a list of current medications, and have any recent imaging (CT, MRI, PET) handy. You’ll also be asked to lie still on a flat table while the scanner captures images.
Radiation therapy can be a powerful ally in the fight against myeloma when used for the right reasons. By understanding the process, asking clear questions, and staying on top of side‑effect management, you put yourself in the best possible position to live well while the disease is under control.




Valerie Vanderghote
October 17, 2025 AT 01:50When you first hear about radiation for myeloma it can feel like a foreign language invading your personal space. I remember sitting in the simulation room and feeling every photon as a tiny whisper against my skin. The pain of a bone lesion is already heavy enough, and adding a machine that sounds like a sci‑fi bomber only amplifies the anxiety. It helps to think of the treatment as a focused spotlight rather than a blanket, targeting the exact spot that hurts you the most. Keep in mind that the side effects stay local, so you’re not signing up for a body‑wide storm.
Michael Dalrymple
October 19, 2025 AT 09:23Radiation therapy in multiple myeloma serves a highly specific purpose within the broader therapeutic regimen.
Its primary function is palliation, aimed at alleviating localized bone pain that systemic agents may not fully address.
By delivering high‑energy photons to a well‑defined target, clinicians can achieve tumor control while sparing surrounding healthy tissue.
The planning phase begins with a CT simulation, which creates a three‑dimensional representation of the lesion.
In many cases an MRI is incorporated to enhance soft‑tissue contrast, allowing for more precise contouring.
The radiation oncologist then collaborates with physicists to calculate optimal beam angles and dosimetric parameters.
When a curative intent is not feasible, a palliative dose such as 8 Gy in a single fraction may be selected to provide rapid relief.
Alternatively, fractionated schedules of 20 Gy over five sessions or 30 Gy over ten sessions are employed for more extensive disease.
Side effects remain largely confined to the treatment field, manifesting as skin erythema, fatigue, or transient pain flare.
Patients with large marrow volumes exposed to radiation should be monitored for hematologic suppression, as blood counts may dip temporarily.
The integration of radiation with systemic therapies requires careful timing to avoid additive toxicities, especially skin reactions.
Importantly, radiation does not replace systemic chemotherapy, immunotherapy, or stem‑cell transplantation; it complements them.
Discussions with the multidisciplinary team should address expectations, potential benefits, and the realistic goals of treatment.
Proactive skin care, adequate hydration, and gentle activity can mitigate many of the mild adverse effects.
Ultimately, understanding the role of radiation empowers patients to make informed decisions and maintain quality of life throughout their disease course.
Richard O'Callaghan
October 21, 2025 AT 16:57The simlation appt is where they map out the spot you need to hit. I always bring my phone so I can take notes while the techs move the machine around. Make sure the doc checks the dose numbers twice, typos can mess up the plan.
Alexis Howard
October 24, 2025 AT 00:30Radiation is not a cure it just hits the bad spot fast you feel the burn then the relief
Steve Holmes
October 26, 2025 AT 07:03Wow, the side‑effects list is surprisingly short, isn’t it?, and that’s a huge win, especially when you’re juggling chemo, steroids, and daily life!, keep that moisturizer handy, and stay hydrated, it really does make a difference!
Tom Green
October 28, 2025 AT 14:37I’ve seen patients bounce back after a single 8 Gy session; the quick fix can be a game‑changer, yet it’s crucial to keep an eye on bloodwork if the field overlaps marrow, so keep those labs coming.
Frank Diaz
October 30, 2025 AT 22:10Consider this: radiation is a laser‑like focus that carves away the pain, not a blanket that smothers the whole disease. When the beam hits, the tumor cells in that slice of bone are bombarded, losing their ability to divide. This localized annihilation spares the rest of your marrow, which remains available for systemic drugs. Yet the irony is that the very act of concentrating energy can stir an inflammatory response, giving you a brief flare before the calm. That’s why you’ll hear about “pain flare” right after the first fraction. Keep a log of your sensations; it helps the team adjust the schedule if needed. In the grand scheme, radiation is a strategic ally, a precise strike in a war where the enemy is scattered. The true victory lies in preserving the quality of each day you live.
Russell Abelido
November 2, 2025 AT 05:43Thank you for sharing this, it really clears up a lot of confusion! I’ve always felt a little lost when my oncologist mentioned “simulation” – now I get that it’s just a fancy way of mapping the battlefield. It’s reassuring to know the side‑effects stay local, especially the skin stuff; I’ll definitely keep that moisturizer on standby :) Also, staying hydrated sounded like simple advice, but it actually makes a huge difference in how tired I feel after each session. Keep the info coming, it’s gold for patients like us!
lisa howard
November 4, 2025 AT 13:17When I first walked into the radiation suite, I felt like I was stepping onto a movie set, lights blinking, machines humming like giant alien insects. The technical jargon – CT simulation, dosimetry, linear accelerator – swirled around me, each term a tiny vortex pulling my thoughts apart. I tried to stay grounded, reminding myself that this is a targeted strike against a single painful lesion, not a full‑scale war on my whole body. The nurses whispered soothing words, yet the metallic clang of the LINAC still echoed in my mind like a distant drumbeat of war. In that moment, I realized that courage isn’t the absence of fear, but the willingness to sit still under that beam and trust the experts. So I breathed, I focused, and I let the radiation do its precise work.
Cindy Thomas
November 6, 2025 AT 20:50Honestly, the whole “radiation is just a side‑effect manager” line feels oversimplified; there’s more nuance, especially when you consider bone‑seeking isotopes that travel systemically. Still, I appreciate the practical tips – moisturize, hydrate, watch for swelling – they’re the real takeaways. It’s easy to get lost in the technical speak, but breaking it down into daily habits makes it manageable 😊. The balance between aggressive treatment and quality of life is a tightrope, and sharing these details helps keep that rope steady.
Kate Marr
November 9, 2025 AT 04:23Listen, we can’t let foreign‑born scientists dictate how we treat our own bodies! 🇺🇸 Radiation should only be used when it serves America’s best interests, and any “systemic” approach feels like surrendering to globalist agendas. The table you posted shows the obvious truth – local therapy keeps the fight at home, while chemo spreads the mess worldwide. Let’s stay vigilant, protect our marrow, and demand that every dose be vetted by a truly American board of experts!
James Falcone
November 11, 2025 AT 11:57Radiation’s a tool, not a miracle; use it wisely and keep your eyes on the bigger battle.
Sara Werb
November 13, 2025 AT 19:30Wow!!! The whole thing sounds like a secret government experiment!!! They’re putting radiation in our bones and we’re just supposed to trust the “doctors”!!! 🌟 I’m telling you, the real side‑effects are hidden, and they don’t want us to read the fine print!!! Stay alert, stay skeptical, and don’t let them push a one‑size‑fits‑all plan onto you!!!
Winston Bar
November 16, 2025 AT 03:03Radiation is just another fad, another thing to hype up for pharma profit. You think a few Gy will fix everything? Nah, it’s a band‑aid that doesn’t address the root. Keep your expectations low and your skepticism high.
Lauren Sproule
November 18, 2025 AT 10:37i think this guide is really helpful and i appreciate the clear steps, the tips about skin care are especially good, its nice to have practical advice not just medical jargon, thanks for sharing the info.
CHIRAG AGARWAL
November 20, 2025 AT 18:10Yo, radiation’s just a quick fix, but make sure you’re not missing the bigger picture!
genevieve gaudet
November 23, 2025 AT 01:43The guide ties together the technical and practical aspects nicely.