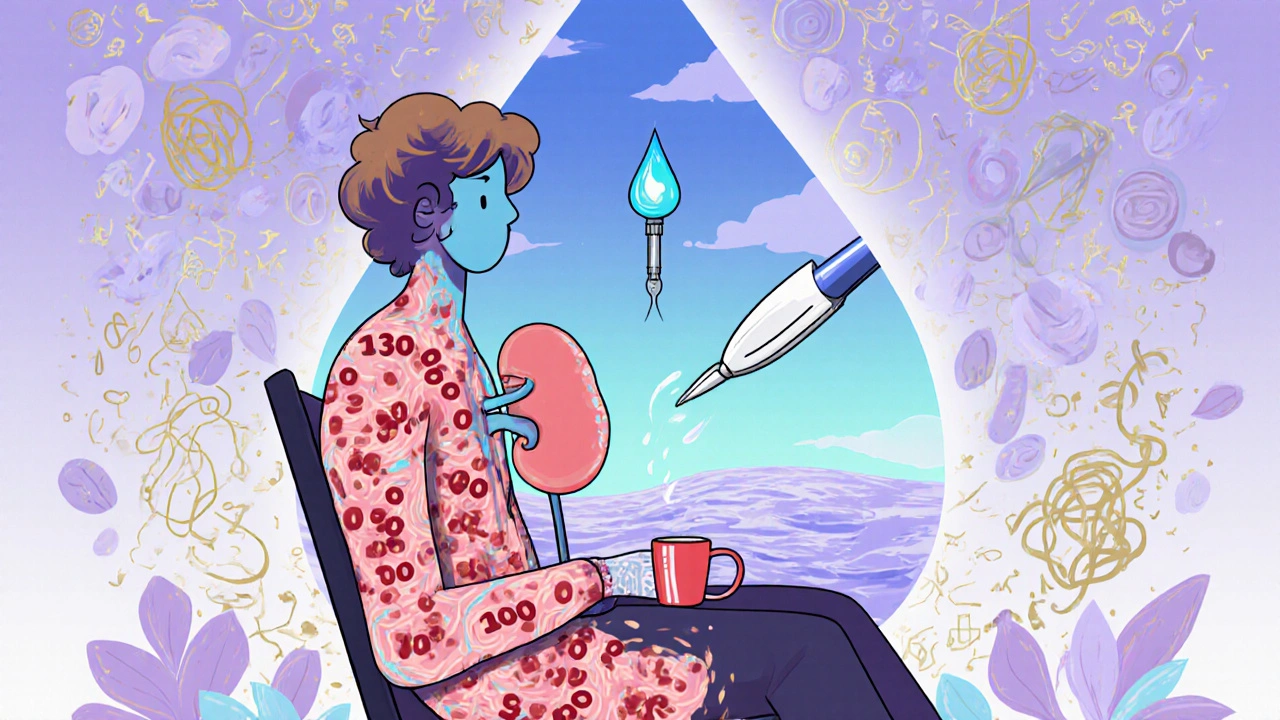
Polycystic kidney disease (PKD) isn’t just about fluid-filled sacs in the kidneys. It’s a genetic time bomb that slowly destroys kidney function over decades. If you have PKD, your kidneys can grow to three times their normal size, weighing up to 30 pounds - all because of faulty genes passed down from a parent or, in rare cases, appearing out of nowhere. Around 600,000 people in the U.S. live with this condition, and nearly half of them will need dialysis or a transplant by age 60. The good news? You don’t have to wait for kidney failure. There are proven ways to slow it down - if you know what to look for and when to act.
What Exactly Is Polycystic Kidney Disease?
PKD is a hereditary condition where cysts - fluid-filled sacs - form in the kidneys and keep growing. These aren’t harmless bumps. Over time, they crowd out healthy tissue, reduce blood flow, and make the kidneys work harder until they eventually fail. The disease is split into two main types: autosomal dominant polycystic kidney disease (ADPKD) and autosomal recessive polycystic kidney disease (ARPKD). ADPKD makes up more than 98% of all cases. It’s the kind you inherit from just one parent. ARPKD is rare, often shows up in babies or young children, and requires mutations from both parents.
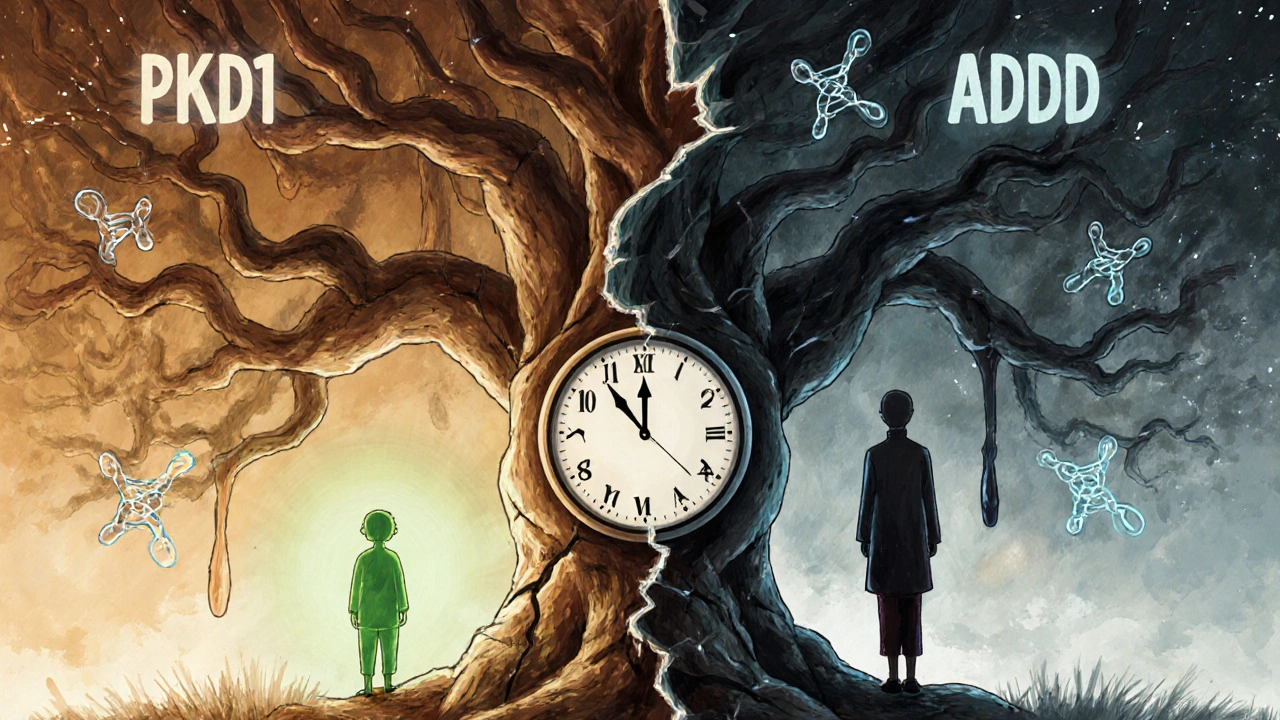
The genes behind ADPKD are well mapped: PKD1 causes about 78% of cases and tends to be more aggressive. PKD2 accounts for 15% and usually leads to slower disease progression. If you have a PKD1 mutation, you’re more likely to need dialysis by your 50s. With PKD2, many people don’t reach kidney failure until their 70s or later. About 10% of ADPKD cases happen without any family history - a brand-new mutation. That means even if no one in your family has it, you could still carry the gene.
How Do You Know If You Have It?
Symptoms don’t always show up early. Many people feel fine until their 30s or 40s. But when they do appear, they’re hard to ignore. High blood pressure is the most common early sign - often the first clue doctors spot. Chronic pain in the back or sides, blood in the urine, frequent kidney infections, and swelling in the abdomen are all red flags. The PKD Foundation’s 2023 survey found that 78% of patients struggle with ongoing pain, and 65% say it’s moderate to severe.
Diagnosis isn’t guesswork. If you have a family history and are over 30, doctors look for at least 10 cysts in each kidney using an ultrasound. For younger people or those without a clear family history, a CT scan or MRI might be needed. Genetic testing is now affordable - around $1,200 - and can confirm whether you carry PKD1 or PKD2 mutations. It’s especially useful if you’re planning to have kids or if your symptoms don’t fit the usual pattern.
ADPKD vs. ARPKD: Key Differences
These aren’t just two versions of the same disease - they’re fundamentally different in how they behave.
- ADPKD: Starts in adulthood. Symptoms usually show up between ages 30 and 40. Kidney failure typically happens by age 60-70. One faulty gene copy is enough to trigger it. You inherit it from one parent.
- ARPKD: Starts in infancy or early childhood. Babies may be born with enlarged kidneys and breathing problems. Liver damage often goes hand-in-hand with kidney issues. Both parents must carry the PKHD1 gene mutation. Each child has a 25% chance of getting it.
ARPKD is far less common - about 1 in 20,000 births - but it’s more dangerous in early life. About 30% of newborns with ARPKD don’t survive past their first month. Those who do often face lifelong liver complications. ADPKD, while slower, is far more widespread. It’s the fourth leading cause of kidney failure in the U.S., accounting for 2% of all cases.
How Is It Managed Today?
There’s no cure - yet. But there are powerful tools to delay kidney failure. The goal isn’t to remove cysts. It’s to protect what’s left of your kidney function.
Control your blood pressure. This is the single most important step. Keeping it below 130/80 mmHg can slow cyst growth and kidney damage. ACE inhibitors or ARBs are the go-to medications. One patient shared on a kidney forum: “Starting blood pressure meds at 28 kept my kidney function at 65% at age 45.” That’s not luck - that’s science.
Use tolvaptan (Jynarque). Approved by the FDA in 2018, this is the first drug proven to slow the progression of ADPKD. It works by blocking a hormone that makes cysts grow. In a major clinical trial, it reduced kidney function decline by 1.3 mL/min per year. But it’s expensive - about $115,000 a year - and can cause serious side effects like liver damage. It’s only for people with rapidly progressing disease, confirmed by imaging and eGFR decline.
Monitor kidney function. Get your eGFR tested at least once a year. Once it drops below 60 mL/min/1.73m², testing should go to every three months. Tracking total kidney volume with MRIs every 1-3 years helps predict how fast the disease is moving.
Manage symptoms. Pain is common. Over-the-counter painkillers like acetaminophen are safer than NSAIDs (ibuprofen, naproxen), which can hurt kidneys. Drink plenty of water - it may help slow cyst growth. Avoid caffeine and high-salt diets. Quit smoking. These aren’t just lifestyle tips - they’re part of your treatment plan.
What’s on the Horizon?
Research is moving fast. The HALT-PKD study showed that pushing blood pressure even lower - to 110/75 mmHg - slowed kidney growth by 14.2% over five years. That’s a game-changer for high-risk patients.
New drugs are in phase 3 trials. Lixivaptan, a cousin of tolvaptan, is expected to complete testing in 2024. Bardoxolone methyl showed a 4.9 mL/min higher eGFR at 48 weeks compared to placebo in early studies. These aren’t cures, but they’re steps toward stopping the disease before it reaches dialysis.
Gene therapy and CRISPR-based approaches are still in early labs, but the fact that we’ve pinpointed PKD1 and PKD2 means we now have real targets. The PKD drug market is projected to hit $2.8 billion by 2028 - not because of hype, but because real patients need real solutions.
The Emotional Toll and Real-Life Challenges
Living with PKD isn’t just physical. The uncertainty is exhausting. One Reddit user wrote: “It took seven years and three doctors to get my ADPKD diagnosis - even though my dad had it.” Delayed diagnosis is common. Many people are told they have “just back pain” or “high blood pressure from stress.”
63% of surveyed patients report anxiety about kidney failure. That’s not paranoia - it’s rational. With a 75% chance of needing dialysis or transplant by age 70, the future feels heavy. But community support helps. Patients who join PKD Foundation groups report better coping skills and faster access to new treatments.
Financial stress is real too. Annual healthcare costs for ADPKD average $45,300 - and jump to $95,700 in the year before dialysis. Medicare spends 5% of its end-stage renal disease budget on PKD patients, even though they make up only 2% of cases. Why? Because they’re younger. They need treatment longer.
What Should You Do Next?
If you have a family history of PKD:
- Get screened with an ultrasound by age 30, even if you feel fine.
- Check your blood pressure regularly - at home and at the doctor’s.
- Ask your doctor about eGFR testing and whether genetic testing is right for you.
- If you’re diagnosed, start blood pressure meds immediately - don’t wait for symptoms.
- Connect with the PKD Foundation. They offer free resources, support groups, and updates on clinical trials.
If you don’t have a family history but have unexplained high blood pressure, chronic back pain, or blood in your urine - get checked. PKD doesn’t always come with a family tree. New mutations happen. And catching it early can change your life.
PKD isn’t a death sentence. It’s a chronic condition - one that can be managed, slowed, and sometimes even delayed for decades. The tools are here. The knowledge is here. What’s missing is the urgency to act before it’s too late.
Can polycystic kidney disease be cured?
No, there is currently no cure for polycystic kidney disease. Treatments focus on slowing disease progression, managing symptoms like high blood pressure and pain, and delaying kidney failure. The only way to replace failed kidneys is through transplantation. Research into gene therapies and new drugs is ongoing, but none have reached the stage of being a cure.
Is PKD inherited from the mother or father?
It depends on the type. For ADPKD, which is the most common form, you only need to inherit one faulty gene from either parent - mother or father - to develop the disease. For ARPKD, you must inherit two faulty copies of the gene, one from each parent. So both parents must be carriers, even if neither has symptoms.
How do I know if my children will inherit PKD?
If you have ADPKD, each child has a 50% chance of inheriting the mutated gene. Genetic testing can identify whether a child carries the mutation, even before symptoms appear. For ARPKD, both parents must be carriers. In that case, each child has a 25% chance of having the disease, a 50% chance of being a carrier, and a 25% chance of not inheriting the mutation at all. Prenatal or preimplantation genetic testing is available for families with known mutations.
Does drinking water help with PKD?
Yes, staying well-hydrated may help slow cyst growth. Studies suggest that high fluid intake reduces vasopressin levels - a hormone that promotes cyst expansion. While it won’t stop the disease, drinking 3-4 liters of water daily, especially if you’re not on fluid restrictions, is often recommended by nephrologists as a simple, low-risk way to support kidney health.
What foods should I avoid with PKD?
Avoid high-sodium foods, processed meats, canned soups, and salty snacks - salt raises blood pressure and worsens kidney damage. Limit caffeine, as it may increase cyst growth. If kidney function declines, you may also need to restrict potassium and phosphorus. Always work with a renal dietitian to tailor your diet to your stage of disease.
When should I start seeing a nephrologist?
As soon as you’re diagnosed, even if you feel fine. A nephrologist specializes in kidney disease and can monitor your eGFR, kidney size, and blood pressure trends over time. They can also determine if you’re a candidate for tolvaptan or other emerging therapies. Early specialist care is linked to slower disease progression and better long-term outcomes.




fiona collins
November 24, 2025 AT 21:15Just got my ultrasound results-12 cysts in each kidney. I’m 34. No symptoms yet, but I started lisinopril this week. Drinking 3.5L of water daily. No caffeine. No salt. It’s not glamorous, but it’s my new routine.
Srikanth BH
November 26, 2025 AT 05:14You’re not alone. I was diagnosed at 29. My eGFR’s still at 72 at 41. Tolvaptan’s expensive, but my insurance covered it after three appeals. Stay consistent. Small steps add up. You’ve got this.
Josh Zubkoff
November 26, 2025 AT 07:55Let’s be real-this whole PKD thing is a corporate scam. They sell you blood pressure meds, then tolvaptan at $115k a year, then tell you to drink water like it’s some miracle cure. Meanwhile, Big Pharma’s laughing all the way to the bank. They don’t want a cure-they want lifelong customers. And don’t get me started on genetic testing being $1200. Who can afford that? The system is rigged. I’ve got PKD1, and I’m not taking any of their drugs. I’m going herbal. Turmeric, milk thistle, and a strict keto diet. My nephrologist hates me, but my labs are stable. Coincidence? I think not.
Timothy Sadleir
November 27, 2025 AT 23:06While I appreciate the anecdotal nature of your claims, Mr. Zubkoff, it is imperative to emphasize that the clinical efficacy of herbal interventions in ADPKD has not been validated in any randomized, double-blind, placebo-controlled trial. The pharmacokinetic profile of curcumin, for instance, demonstrates negligible bioavailability without adjuvants such as piperine-further undermining its therapeutic utility. The FDA approval of tolvaptan was predicated upon the TEMPO 3:4 trial, which demonstrated a statistically significant reduction in total kidney volume growth rate (p<0.001). To reject evidence-based medicine in favor of unregulated supplements constitutes a breach of the duty of care owed to one’s own health.
Jennifer Griffith
November 28, 2025 AT 19:08lol i got the test done and they said i had pdk1 but i think they messed up my file. my dad never had it so how am i even a thing??
prasad gaude
November 30, 2025 AT 08:02In India, we say: ‘The body is a temple, but the genes are the architects.’ I was diagnosed at 37. No family history. My kidneys are already 2.5x normal size. But I meditate every morning. I walk 8 km daily. I eat only what my grandmother cooked-no processed food, no sugar, no soda. I don’t believe in drugs. I believe in rhythm. The body remembers. It knows how to heal-if you stop screaming at it.
Roscoe Howard
November 30, 2025 AT 23:02It’s no surprise that the U.S. has 600,000 cases. We’ve been poisoning our water with fluoride and our food with high-fructose corn syrup for decades. This isn’t genetic-it’s environmental. And now they want to charge us $115,000 to fix it? Meanwhile, China and India have lower PKD rates because they don’t eat our garbage. Wake up, Americans. This isn’t medicine-it’s colonization by pharmaceuticals.
Pallab Dasgupta
December 1, 2025 AT 03:28I’ve seen people with PKD live to 80 without dialysis. I’ve seen others crash by 45. It’s not just the gene-it’s your life. I lost my brother to this. He smoked, drank, ate chips, ignored his BP. I don’t smoke. I don’t drink. I drink water like it’s oxygen. I track my numbers like a hawk. You don’t fight PKD with hope. You fight it with discipline. One day at a time.
Kimberley Chronicle
December 1, 2025 AT 05:25From a nephrology research perspective, the emerging data on lixivaptan is promising-particularly in patients with rapid eGFR decline (≥5 mL/min/yr). The phase 3 trial (NCT04895165) shows a 22% reduction in TKV growth vs. placebo at 18 months. Also, the 2024 HALT-PKD extension cohort suggests that sustained BP <110/75 correlates with delayed onset of ESRD by 8.7 years. Early intervention is key-ideally before eGFR drops below 80.
Sharley Agarwal
December 2, 2025 AT 18:58Of course you feel fine now. That’s what they all say. Until one day, you’re on dialysis. And then? You’re just a statistic. Don’t be naive. You think water helps? Please. It’s a placebo for people who can’t afford the truth.
Archana Jha
December 3, 2025 AT 10:29wait so if i have pdk1 and my kid gets it too does that mean the government is putting it in the water? or is it the vaccines? i heard the mRNA shots change your dna. my cousin’s kid got pkd after the shot. they dont want us to know. the cdc hides the data. i checked the patent for tolvaptan-it was funded by the same company that made the flu shots. its all connected.
Rachel Villegas
December 4, 2025 AT 14:02I’m the author of this post. Thank you for all the thoughtful responses. I was diagnosed at 31. I’m on tolvaptan. My kidneys are growing, but slower. I started a support group last month-12 people, all from Reddit. We meet every Sunday. If you’re out there reading this and feeling alone-you’re not. We’re here. And we’re not giving up.