COPD Inhaler: Types, Safety, and How to Use Them Right
When you have COPD inhaler, a handheld device that delivers medication directly to the lungs to open airways and reduce inflammation. Also known as respiratory inhaler, it's one of the most common tools for managing chronic obstructive pulmonary disease. Without proper use, even the best medication won’t help—many people think they’re using it right, but they’re not getting the full dose. The right COPD inhaler can mean the difference between being able to walk across the room or needing oxygen just to sit still.
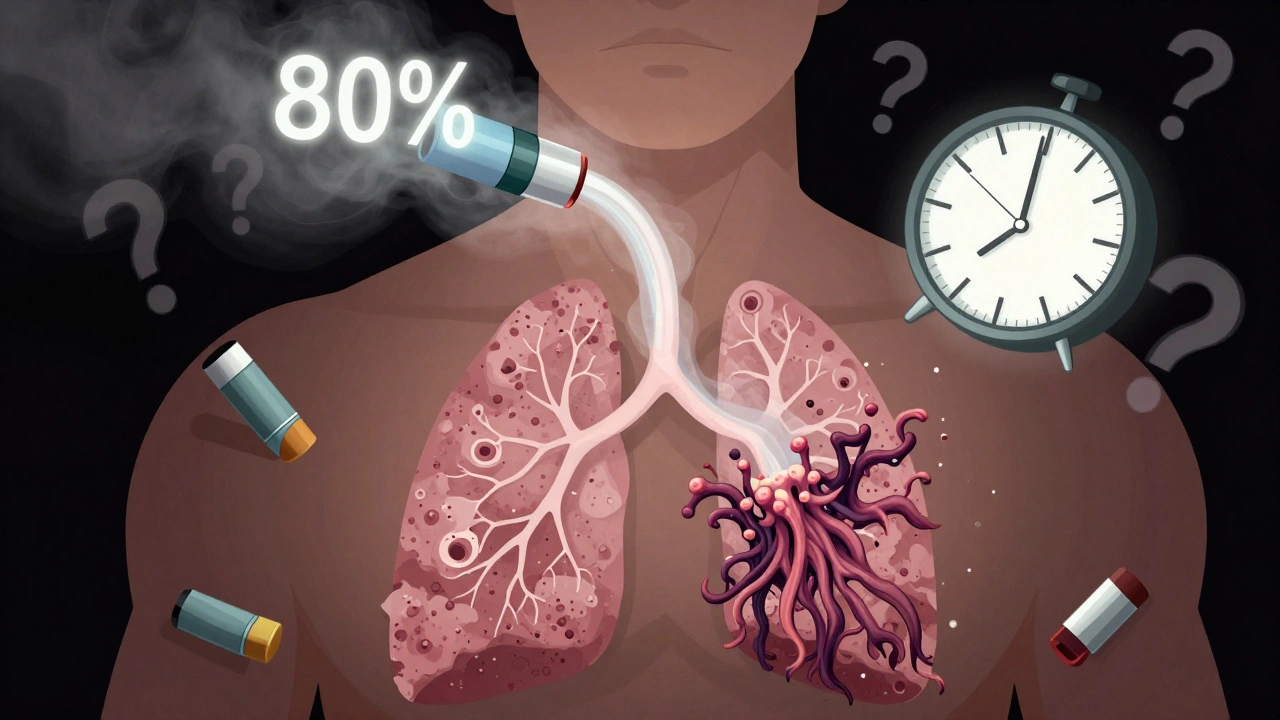
COPD inhalers come in two main types: bronchodilator, medications that relax the muscles around the airways to make breathing easier and corticosteroid inhaler, anti-inflammatory drugs that reduce swelling and mucus in the lungs. Most people need a combination of both. Bronchodilators like albuterol or tiotropium act fast to relieve sudden breathlessness. Corticosteroids like fluticasone or budesonide work over time to prevent flare-ups. But if you don’t shake, prime, or inhale deeply enough, up to 80% of the dose ends up in your mouth or throat—not your lungs.
Using a COPD inhaler correctly isn’t just about technique—it’s about avoiding mistakes that lead to hospital visits. People often skip rinsing their mouth after using steroid inhalers, which can cause thrush. Others switch between brands without realizing the device design changes, making their old technique useless. Even the shape of the mouthpiece matters. Some inhalers need a slow, deep breath; others need a quick, sharp puff. And if you’re using a spacer, are you cleaning it weekly? A dirty spacer traps medication and reduces effectiveness.
These aren’t small details. They’re the difference between feeling better and feeling worse. That’s why patient counseling—like the kind shown in posts about catching dispensing errors—makes such a big difference. A pharmacist asking you to demonstrate your technique can catch a wrong inhaler hold, a missed breath hold, or an expired device before it causes a problem. And if you’ve ever wondered why your generic inhaler feels different, it might not be the active drug—it could be the propellant, the coating, or even the way the metering valve works.
What you’ll find below are real, practical guides from people who’ve been there. You’ll learn how to compare new prescription labels to avoid mix-ups, why generic versions sometimes cause unexpected reactions, and how to talk to your doctor when your inhaler isn’t working like it should. There’s no fluff—just clear steps, common pitfalls, and what actually works when your lungs are struggling to keep up.
About
Medications