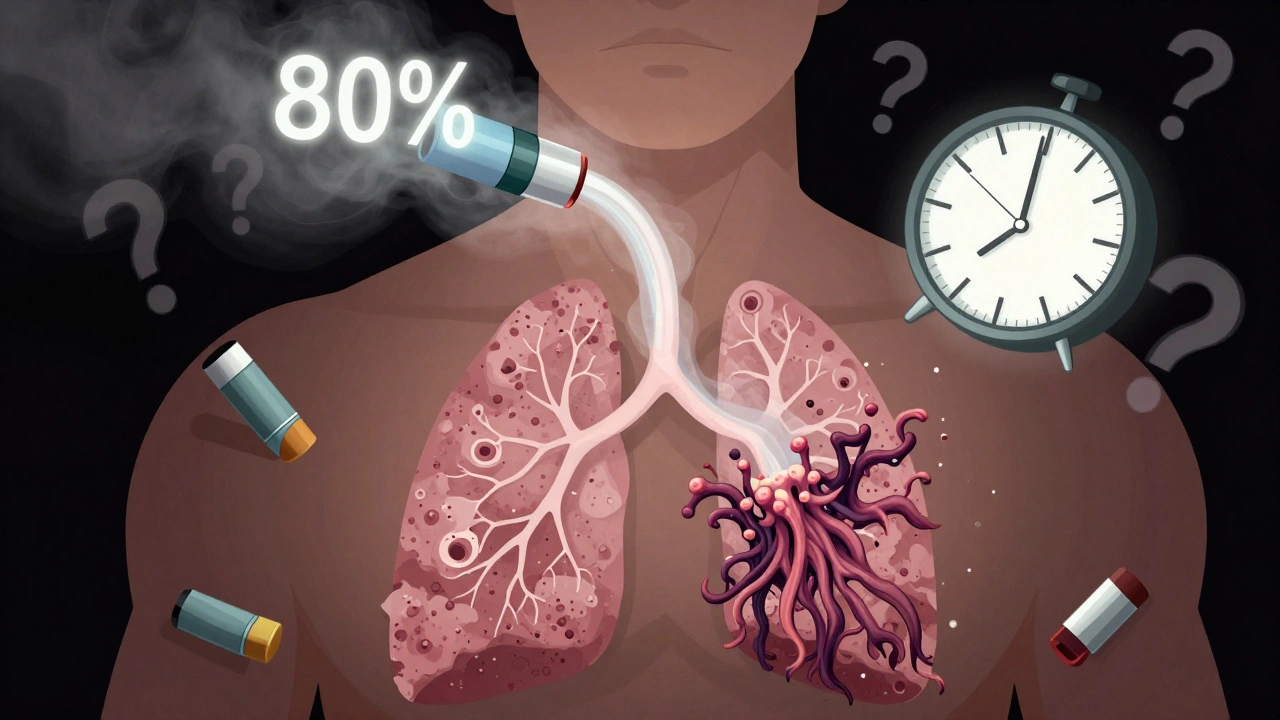
Most people with asthma or COPD use an inhaler every day. But here’s the hard truth: inhaler technique is wrong in 70 to 90% of cases. That means if you’re using your inhaler the way you’ve always done it, you’re probably getting less than 20% of your medication into your lungs. The rest is stuck in your mouth or throat - not helping your breathing, but causing side effects like thrush, hoarseness, or even worsening symptoms.
Why Your Inhaler Isn’t Working Like It Should
Metered-dose inhalers (MDIs) are tiny, pressurized cans that spray medicine into your airways. They’ve been around since the 1950s, but most people still use them wrong. The medicine comes out in a fast puff - about 0.1 to 0.2 seconds - and if you don’t time your breath right, it hits the back of your throat instead of your lungs. That’s why so many people say, "I used my inhaler, but I still feel wheezy." The problem isn’t the medicine. It’s the delivery. Studies show that when technique is correct, up to 80% of the dose reaches the lungs. When it’s wrong? Only 10 to 20%. That’s why your doctor keeps asking you to refill your rescue inhaler every month - not because your asthma is getting worse, but because you’re not getting the full dose.The 8-Step Correct Inhaler Technique
Here’s how to use your inhaler properly - every single time. This applies to standard HFA inhalers like Ventolin HFA, Flovent HFA, Advair HFA, and Symbicort. (Note: Some newer inhalers like QVAR and Alvesco don’t need shaking - check your label.)- Remove the cap. Check for dust or debris inside the mouthpiece. Don’t rinse the mouthpiece with water - it can damage the device.
- Shake the inhaler for 5 to 10 seconds. Most HFA inhalers need this. Shaking less than 5 seconds can reduce the dose by 25 to 40%. If your inhaler hasn’t been used in two weeks, prime it with 2 to 4 test sprays into the air (check your prescription label - Alvesco needs 2, QVAR needs 4).
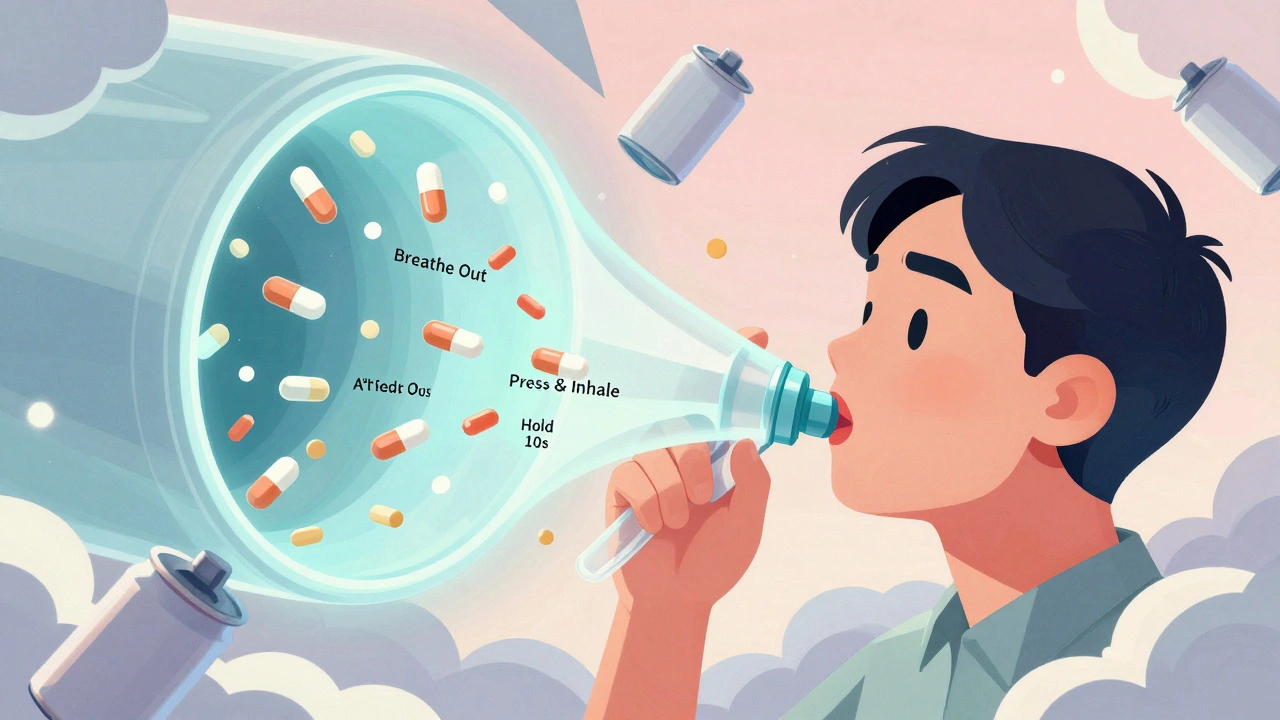
- Breathe out fully. Empty your lungs completely. Don’t breathe out into the inhaler. Just let all the air go.
- Place the mouthpiece between your teeth and seal your lips around it. No gaps. No holding it 1 inch away. This is a common mistake. The spray needs to go directly into your mouth.
- Start breathing in slowly and deeply just before or at the same time as pressing down. This is the hardest part. Press the inhaler and breathe in - not before, not after. If you press first and then breathe, you’ll get a puff of medicine in your mouth. If you breathe in first, you’ll inhale nothing. The goal is to match the puff with the start of your inhale.
- Keep breathing in slowly for 3 to 5 seconds. Don’t take a quick, sharp breath. You need to inhale at about 30 liters per minute. Too fast, and the medicine hits your throat. Too slow, and it doesn’t reach deep enough.
- Hold your breath for 10 seconds. This lets the medicine settle in your airways. Studies show holding for 10 seconds increases lung deposition by 30% compared to just 5 seconds. Count slowly: "one-Mississippi, two-Mississippi..."
- Breathe out slowly through your nose. Then rinse your mouth with water and spit it out - especially if you’re using a steroid inhaler like Flovent or Advair. This cuts your risk of oral thrush by 40%.
What Most People Get Wrong
You’re not alone if you’ve made these mistakes. Here are the top five errors, based on clinical data:- Not exhaling fully before inhaling. 42% of users skip this. If your lungs are already full, you can’t pull in the medicine properly.
- Holding your breath for less than 5 seconds. 63% of patients do this. The medicine needs time to stick to your airway walls.
- Inhaling too fast. 57% of users take a sharp, quick breath. That sends the medicine straight to your throat.
- Forgetting to prime the inhaler. 31% of people don’t prime a new or unused inhaler. That means the first few puffs are just propellant - no medicine.
- Head tilted too far back or forward. 28% of users tilt their head incorrectly. Keep your head level, eyes straight ahead. It helps the medicine flow down into your lungs.
Spacers: The Secret Weapon for Better Delivery
If you struggle with timing - especially if you’re older, have arthritis, or are helping a child - a spacer (also called a holding chamber) is a game-changer. It’s a plastic tube that attaches to your inhaler. You spray the medicine into the spacer, then breathe in slowly from it.- Spacers boost lung delivery from 10-20% to 70-80%.
- You don’t need perfect timing - spray once, then breathe in normally.
- They reduce throat irritation and thrush by trapping large particles before they reach your mouth.
- For kids, use a spacer with a mask. It’s easier than trying to get them to seal their lips around a mouthpiece.
A 2022 study found that people using spacers had 45% fewer asthma attacks than those using inhalers alone. And it’s not expensive - most are under £10 in the UK, and many pharmacies give them out for free with a prescription.
Dry Powder vs. Metered-Dose: Which Is Right for You?
Not all inhalers are the same. There are two main types:| Feature | Metered-Dose Inhaler (MDI) | Dry Powder Inhaler (DPI) |
|---|---|---|
| Medication delivery | Press and breathe slowly | Breathe in fast and deep |
| Inhalation speed needed | 30 liters per minute | 60 liters per minute |
| Best for | Most adults, children, emergency use | People who can take a strong, fast breath |
| Requires shaking? | Yes (except QVAR, Alvesco) | No |
| Needs spacer? | Yes, for better results | No |
| Onset of action | 1-5 minutes | 5-15 minutes |
| Moisture sensitive? | No | Yes - keep dry |
If you can’t take a fast, deep breath - maybe because of COPD, age, or weakness - a DPI won’t work for you. MDIs with spacers are the better choice. If you’re young and healthy, and you can inhale hard and fast, a DPI might be easier. But if you’re unsure, stick with the MDI + spacer combo. It’s the most forgiving and effective for most people.

What to Do If You’re Still Struggling
Even after reading this, if you’re not sure you’re doing it right, here’s what to do next:- Ask your pharmacist to watch you use your inhaler. They see dozens of patients every day. They’ll spot your mistake in seconds.
- Use a placebo inhaler for practice. Your doctor can give you a non-medicated version. Practice the steps until it’s automatic.
- Download a training app. Apps like Propeller Health use sensors to detect your technique and give real-time feedback. They’re 92% accurate.
- Watch a video. The NHS and Asthma UK have short, clear videos on YouTube. Watch one with your inhaler in hand.
- Ask for a spacer. If you haven’t used one, try it. It’s the single easiest upgrade to your treatment.
Don’t wait until you’re in the emergency room because your inhaler "didn’t work." Most of the time, it did - you just didn’t get the dose where it needed to go.
What’s Changing in 2025
By 2025, every prescription inhaler in the UK and US will have a QR code on the box. Scan it with your phone, and you’ll get a short video showing the correct technique for that exact device. That’s because research shows people remember better when they see it done.Some new inhalers now have built-in sensors that track when you use them - and whether you did it right. These "smart inhalers" send alerts to your phone if you forget to inhale slowly or hold your breath. They’re still pricey, but insurance coverage is starting to expand.
The bottom line? Your inhaler isn’t broken. You just need to use it right. And once you do, you’ll notice the difference - fewer symptoms, fewer rescue puffs, and better sleep at night.
How do I know if my inhaler is empty?
Most inhalers have a counter that shows how many doses are left. If yours doesn’t, track how many you’ve used. A standard inhaler has 200 puffs. If you use 2 puffs twice a day, it lasts about 50 days. Once you hit that number, replace it - even if it still sprays. The medicine inside may be gone, but the propellant still works, giving you a false sense of safety.
Can I use my inhaler without shaking it?
Only if the label says so. Most HFA inhalers like Ventolin, Flovent, and Advair need shaking. But QVAR and Alvesco are designed differently - they don’t need shaking. Always check your prescription label or ask your pharmacist. If you skip shaking on a standard inhaler, you might get a weak or uneven dose.
Why do I get a sore throat after using my inhaler?
That’s usually from steroid medicine (like fluticasone or budesonide) sticking to your throat. It’s not an allergy - it’s a side effect. Rinse your mouth with water and spit it out after every use. This cuts your risk of oral thrush by 40%. You can also use a spacer to reduce throat deposition.
Is it okay to use my rescue inhaler every day?
If you’re using your rescue inhaler (like Ventolin) more than twice a week, your asthma isn’t well controlled. That’s a sign you need to start or adjust your daily controller inhaler. Don’t rely on rescue puffs - they treat symptoms, not the underlying inflammation. Talk to your doctor if you’re using it often.
Should my child use a spacer with their inhaler?
Yes - always. Children under 12 can’t coordinate breathing with puffing. A spacer with a mask is the gold standard for kids. It’s safer, more effective, and reduces side effects. Most pediatricians require spacers for children using inhalers. Ask your pharmacy for a child-sized one - they’re often free with a prescription.




Suzanne Johnston
December 8, 2025 AT 11:02So many people think their inhaler is broken when it’s just them using it wrong. I used to be one of them-until my pharmacist made me practice in front of her with a placebo. I thought I was doing fine. Turns out I was puffing like I was trying to blow out birthday candles on a cake. Changed everything. Now I use a spacer. No more thrush. No more panic attacks when I feel a wheeze coming. It’s not magic-it’s mechanics.
Graham Abbas
December 8, 2025 AT 14:07Bro. I used to think the puff was the medicine. Turns out the puff is just the delivery system. The real medicine? The breath after it. I’ve been using my Flovent for 8 years and never held my breath past 3 seconds. I just assumed it worked. Now I’m counting Mississippis like I’m in a meditation app. My lungs feel like they’re finally getting a damn vacation. Thanks for this. Seriously.
Elliot Barrett
December 9, 2025 AT 23:11Wow. Another article telling me I’m doing everything wrong. Can we just get better inhalers instead of making people into breathing athletes? I’m 68. I have arthritis. My hands shake. You want me to time a breath with a puff? Good luck. Why isn’t there a button that just says ‘Breathe now’?
Shubham Mathur
December 10, 2025 AT 08:01Guys you need to understand this is not just about technique its about dignity when you're old and your body is failing you and you have to do 8 steps to get a puff of air that should be simple why do we make health so complicated its not rocket science its breathing why cant the pharma companies just make a device that works with your body not against it
Ryan Brady
December 10, 2025 AT 16:04LMAO at all these people acting like they’re astronauts landing on Mars just to use an inhaler 😂 I mean come on. We’re talking about a tiny canister. If you can’t figure this out after one doctor visit you probably shouldn’t be driving either. Also spacers? That’s for kids and grandmas. Real men use the inhaler straight. 🤡
Delaine Kiara
December 12, 2025 AT 06:54Okay but let’s be real-this whole thing is a scam. The pharmaceutical industry makes BILLIONS off people buying new inhalers every month because they’re told they’re ‘using it wrong.’ Meanwhile, the real issue? The meds are overpriced and under-tested. I’ve been using my Ventolin since 2015. I’ve never had a thrush issue. I don’t rinse. I don’t use a spacer. I breathe in. I live. End of story. Why are we turning basic medicine into a TED Talk?
Gilbert Lacasandile
December 13, 2025 AT 02:46I’m not a doctor but I’ve watched my mom use her inhaler for 15 years and she never did any of this right. She’d shake it, puff, and immediately cough. I thought she was just being dramatic. Then I saw a video where they showed the medicine hitting the back of her throat like a paintball. She started using a spacer last year. She hasn’t been to the ER since. It’s not glamorous. But it works. Just try it. No judgment.
Haley P Law
December 13, 2025 AT 07:38OMG I JUST REALIZED I’VE BEEN USING MY INHALER WRONG FOR 12 YEARS 😭😭😭 I’M CRYING RIGHT NOW I’M SO EMBARRASSED BUT ALSO SO RELIEVED. I’M GOING TO BUY A SPACER TODAY. I’M TELLING EVERYONE. THIS IS THE MOST IMPORTANT THING I’VE LEARNED SINCE I FOUND OUT YOU CAN’T JUST EAT A CUPCAKE AND EXPECT TO BE HEALTHY. #InhalerAwakening
Andrea DeWinter
December 14, 2025 AT 07:22For anyone with COPD or older adults-don’t feel bad if this feels overwhelming. I’m a nurse and I’ve seen patients cry because they think they’re failing. You’re not. The system is. Spacers are free at most pharmacies. Ask for one. Practice with the placebo. Do it in front of a mirror. Your lungs will thank you. And yes, holding your breath for 10 seconds feels weird at first. But so does brushing your teeth. You do it because it matters.
Angela R. Cartes
December 15, 2025 AT 22:02Ugh. Another ‘guide’ from someone who clearly doesn’t live in the real world. I’m on Medicaid. My pharmacy charges $15 for a spacer. The ‘free’ ones are all broken or missing the valve. And don’t get me started on apps-my phone is a 2017 iPhone. I can barely open a PDF. Why is healthcare always designed for people who can afford tech and time? This isn’t empowerment. It’s guilt-tripping with footnotes.
Andrea Beilstein
December 16, 2025 AT 08:43This reminds me of how in some Indigenous cultures, breath is sacred-not a mechanical function to be optimized. We’ve turned something natural into a checklist. I get the science. But when we make patients feel like failures for not mastering 8 steps to breathe… aren’t we missing the point? Maybe the real solution isn’t better technique. Maybe it’s better access. Better meds. Less fear. Less shame. Just… breathe.