Diuretics for Ascites: What Works, What to Watch, and How They Help
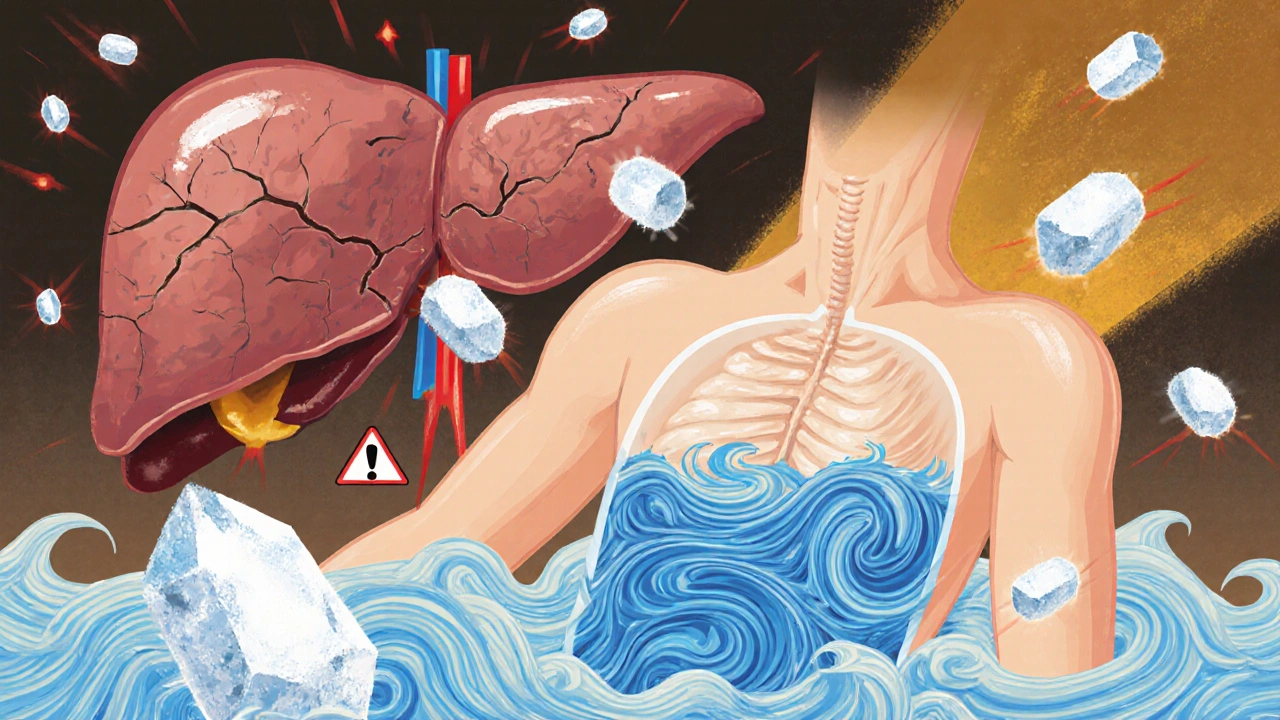
When fluid builds up in the abdomen—known as ascites, an abnormal accumulation of fluid in the peritoneal cavity, often caused by liver disease or heart failure. Also known as abdominal edema, it can make breathing hard, cause discomfort, and signal serious underlying health issues. Diuretics for ascites are one of the most common and effective ways to manage this condition. They don’t cure the root cause, but they help your body get rid of excess fluid, easing pressure and improving quality of life.
Two main types of diuretics are used: spironolactone, a potassium-sparing diuretic that blocks aldosterone, a hormone that causes the body to hold onto salt and water, and furosemide, a loop diuretic that acts quickly on the kidneys to flush out sodium and water. Doctors usually start with spironolactone alone because it works slowly and steadily, reducing the risk of sudden electrolyte imbalances. If that’s not enough, they add furosemide. This combo is the standard for a reason—it’s backed by decades of real-world use in patients with cirrhosis, heart failure, and kidney problems.
But diuretics aren’t magic. They come with risks. Too much can drop your blood pressure, make you dizzy, or cause low potassium or sodium levels. Some people get muscle cramps or feel unusually tired. Monitoring salt intake and checking blood levels regularly is part of the process. You can’t just take these pills and ignore your diet—cutting back on salt is just as important as the medication.
What you won’t find in most doctor’s offices is a one-size-fits-all plan. Some people respond well to low doses. Others need higher amounts or even hospital-based fluid removal. And while these drugs help manage symptoms, they don’t fix the liver damage or heart strain causing the fluid buildup in the first place. That’s why understanding your condition—whether it’s cirrhosis, cancer, or heart failure—is key to knowing what to expect long-term.
Below, you’ll find real-world insights from patients and clinicians on how these drugs are used, what side effects people actually experience, and how to avoid common mistakes. Whether you’re managing ascites yourself or helping someone who is, these posts give you the practical details that aren’t always covered in brochures or quick visits.
About
Medications