When fluid builds up in your abdomen due to liver disease, it’s not just uncomfortable-it’s a warning sign. This fluid buildup, called ascites, happens in about half of people with cirrhosis within 10 years. And once it shows up, your risk of serious complications jumps. About half of these patients won’t survive past two years without proper management. The good news? You can control it. The bad news? The advice you’ve heard might be outdated.
Why Ascites Happens
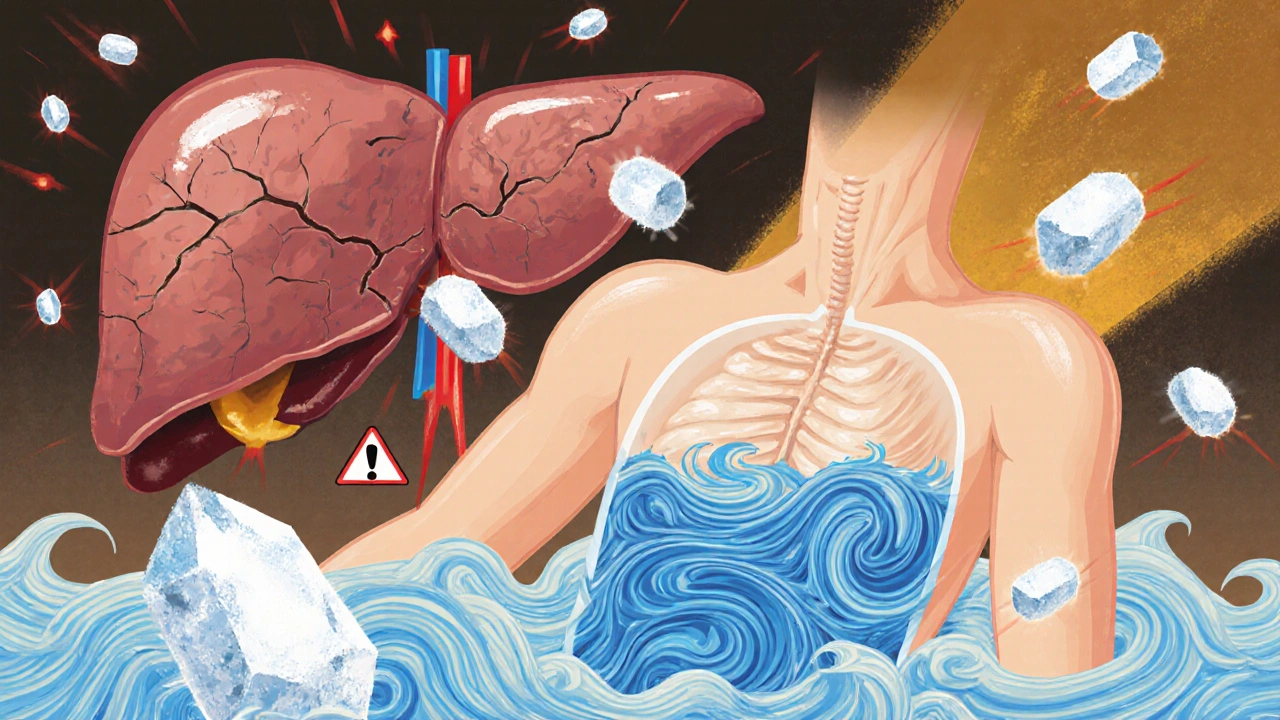
Ascites doesn’t appear out of nowhere. It’s the result of two big problems working together: high pressure in the liver’s blood vessels (portal hypertension) and your kidneys holding onto too much salt and water. When your liver is scarred from cirrhosis, blood can’t flow through it easily. That raises pressure in the portal vein. Your body misreads this as low blood volume and starts flooding your system with hormones that tell your kidneys to keep sodium and water. The result? Fluid leaks into your belly.Sodium Restriction: The Old Rule and the New Debate
For decades, doctors told patients with ascites to cut sodium to less than 2 grams a day. That’s about 5 grams of salt-less than a teaspoon. The idea was simple: less salt means less fluid retention. But here’s the twist: recent studies are challenging this. A 2022 study in Gut and Liver Journal found that patients on a moderate sodium diet (5-6.5 grams of salt daily) had better results than those on strict restriction. Their ascites resolved in 45% of cases, compared to just 16% in the low-sodium group. They also needed fewer procedures to drain fluid. Why? Because going too low may hurt your kidneys. Severely restricting sodium can drop blood pressure in the kidneys, making it harder for them to filter waste. That raises the risk of hepatorenal syndrome-a life-threatening kidney failure that affects up to 35% of patients on ultra-low sodium diets, up from 18% normally. So what’s the real target? Experts now suggest a middle ground: aim for 2-3 grams of sodium daily (about 5-7 grams of salt). That’s enough to help without pushing your kidneys into crisis. The American Association for the Study of Liver Diseases still recommends under 2 grams, but even they warn that strict limits can lead to malnutrition-something that affects up to 90% of cirrhotic patients.Diuretics: The Workhorses of Ascites Treatment
Sodium restriction alone isn’t enough. Most people need diuretics-medications that make your kidneys flush out extra salt and water. The first-line drug is spironolactone. It blocks the hormone aldosterone, which is overactive in cirrhosis and causes salt retention. Doctors start with 100 mg daily, then increase by 100 mg every 3 days, up to 400 mg if needed. It’s slow-acting but gentle on the kidneys. If that’s not enough, they add furosemide, a faster-acting diuretic. Start at 40 mg daily, max 160 mg. The combo works better than either alone. Together, they can help you lose up to 1 kg (2.2 lbs) per day if you have swelling in your legs, or 0.5 kg (1 lb) if you don’t. But there’s a catch. Losing weight too fast can be dangerous. Rapid fluid loss can cause low blood pressure, kidney damage, or electrolyte imbalances. That’s why doctors check your blood sodium levels at least twice a week when you start treatment. If your sodium drops below 130 mEq/L, you may need to adjust fluids or cut back on diuretics.
What Not to Take
Some common medications can make ascites worse. Avoid NSAIDs like ibuprofen or naproxen-they reduce blood flow to the kidneys. ACE inhibitors and ARBs (used for blood pressure) are also risky. Studies show cirrhotic patients on these drugs are 2.3 times more likely to develop end-stage kidney disease. Even over-the-counter supplements can be dangerous. Herbal remedies like licorice root can mimic aldosterone and worsen fluid retention. Always check with your doctor before taking anything new.When Diuretics Don’t Work
About 5-10% of people with ascites don’t respond to maximum doses of diuretics. This is called refractory ascites. Survival for these patients drops to about 50% at 6 months. The go-to treatment? Large-volume paracentesis-draining 5 liters or more of fluid from the belly in one session. But you can’t just drain and forget. You need albumin (a blood protein) given intravenously to prevent a dangerous drop in blood pressure. The rule: 8 grams of albumin for every liter of fluid removed. This works fast and safely, but it’s not a cure. Fluid comes back, often within weeks. That’s why it’s reserved for those who don’t respond to drugs.What About Vaptans?
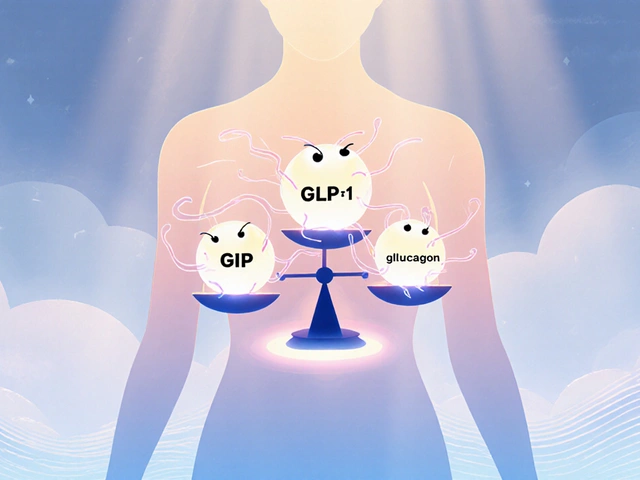
Drugs like tolvaptan (a vaptan) block water retention by targeting vasopressin. Sounds perfect, right? But they’re expensive-$5,000 to $7,000 per course-and limited to 30 days of use. They’re also risky if you’re already low on sodium. Most guidelines don’t recommend them for routine use.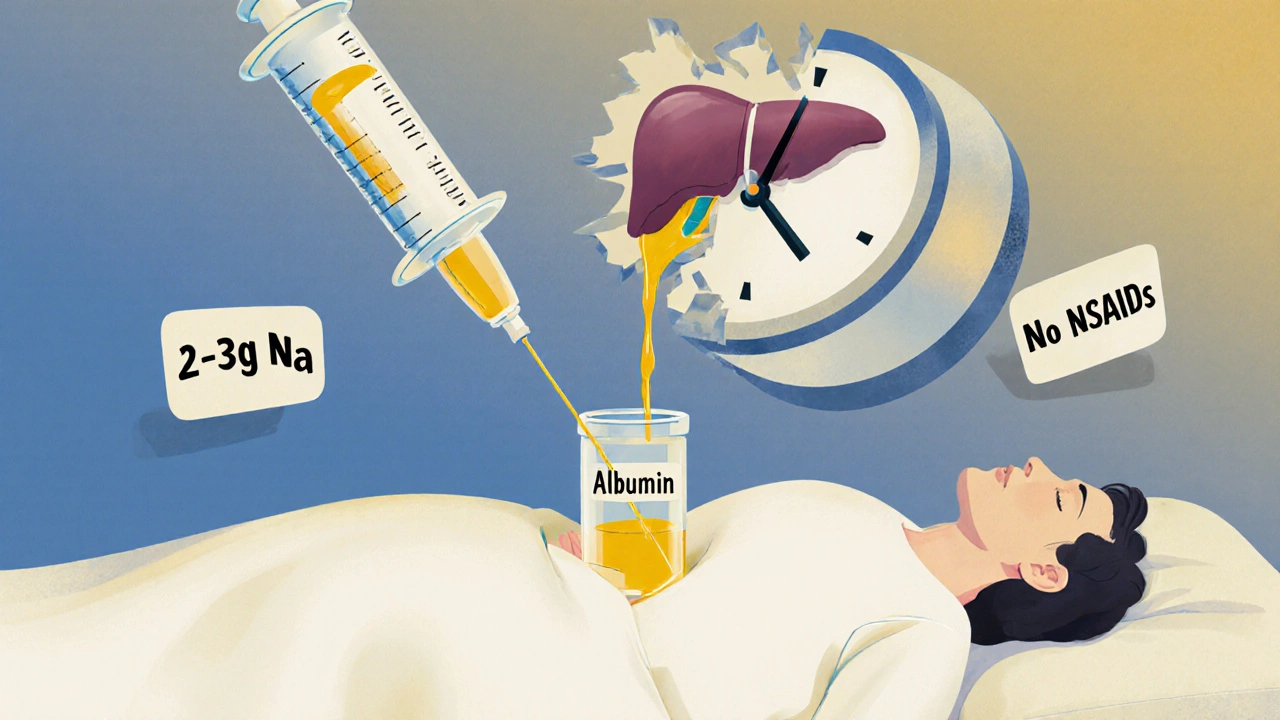
Real-World Challenges
Here’s the truth: sticking to a 2-gram sodium diet is nearly impossible. About 75% of sodium in your diet comes from packaged foods-bread, soup, sauces, deli meats-not the salt shaker. Trying to avoid all of it leads to frustration, poor adherence, and sometimes malnutrition. A 2021 study found fewer than 40% of patients could stick to strict sodium limits. That’s why many hepatologists now personalize treatment. If you’re eating well, staying hydrated, and responding to diuretics, maybe you don’t need to be on a hospital-grade diet.What’s Next?
The big question-how much sodium is safe?-is finally being studied. The PROMETHEUS trial (NCT04567890) is comparing unrestricted versus restricted diets in cirrhosis patients. Results are expected by late 2025. Until then, the best approach is balanced: use diuretics as directed, aim for moderate sodium restriction (2-3 grams daily), avoid kidney-harming drugs, and monitor your weight and blood tests closely. Work with your doctor to find the sweet spot between control and quality of life.Key Takeaways
- Ascites is a sign of advanced liver disease and needs active management.
- Strict sodium restriction (<2 g/day) may do more harm than good for some patients.
- 2-3 grams of sodium per day (5-7 g salt) is now a safer, more realistic target.
- Spironolactone is first-line; furosemide is added if needed.
- Never lose more than 1 kg/day if you have leg swelling, or 0.5 kg/day if you don’t.
- Avoid NSAIDs, ACE inhibitors, and ARBs-they can damage your kidneys.
- Large-volume paracentesis with albumin is the go-to for refractory ascites.
- Diuretics work best when paired with realistic dietary changes, not extreme restrictions.
Can I still eat salt if I have ascites?
Yes-but not too much. Avoid adding salt at the table, but you don’t need to live on plain rice and boiled chicken. Aim for 2-3 grams of sodium daily. That means choosing fresh foods over packaged ones, reading labels, and avoiding processed meats, canned soups, and salty snacks. A moderate approach works better than extreme restriction for most people.
How long does it take for diuretics to reduce ascites?
You’ll usually see results within 3-5 days, but it can take up to 2 weeks to reach full effect. Spironolactone works slowly, so don’t get discouraged if you don’t lose weight right away. Your doctor will adjust your dose based on your weight, urine output, and blood tests.
What happens if I stop taking my diuretics?
Fluid will come back-often quickly. Stopping diuretics without medical supervision can lead to rapid fluid buildup, increased abdominal pressure, breathing trouble, and higher risk of infection. Always talk to your doctor before making changes.
Can ascites be cured?
Not really-not until the underlying liver damage is reversed. In most cases, ascites is a sign that cirrhosis has progressed. Treatment controls the fluid but doesn’t fix the liver. The only cure for advanced cirrhosis is a liver transplant. Until then, the goal is to manage symptoms and avoid complications.
Is drinking less water helpful for ascites?
Only if you have low blood sodium (hyponatremia). For most people with ascites, drinking normal amounts of water is fine and even important. Restricting fluids too much can worsen kidney function and increase the risk of dehydration. Your doctor will tell you if you need to limit fluids based on your blood tests.
What foods should I avoid with ascites?
Avoid processed foods: canned soups, frozen meals, deli meats, pickles, soy sauce, chips, and fast food. Also skip salted butter, cheese, and bread with added salt. Choose fresh fruits, vegetables, lean meats, and plain grains. Cook at home when you can-this is the best way to control sodium.
How do I know if my ascites is getting worse?
Watch for rapid weight gain (more than 1 kg in 2 days), increased abdominal size, trouble breathing when lying flat, swelling in your legs or ankles, or feeling unusually tired. If you notice any of these, contact your doctor. Early intervention prevents complications like infection or kidney failure.


Jordyn Holland
November 28, 2025 AT 09:59Oh wow, another medical article pretending to be revolutionary because it dares to suggest we might not be torturing patients with salt-free bread. Newsflash: people aren’t robots. You can’t force someone with cirrhosis to live on steamed kale and distilled water and expect them to not spiral into depression, malnutrition, or just quit altogether. The real villain here isn’t sodium-it’s the medical industry’s obsession with arbitrary numbers that ignore human reality.
And let’s be real-2 grams of sodium? That’s less than what’s in a single packet of soy sauce. Who even eats like that? I’ve seen patients cry in clinic because their grandkids’ birthday cake was ‘off-limits.’ This isn’t medicine. It’s moral policing with a stethoscope.
Also, why is no one talking about how the AASLD clings to outdated guidelines like they’re holy scripture? They’re not wrong to warn about malnutrition-they just don’t have the guts to admit their own guidelines are part of the problem.
Meanwhile, the liver transplant waiting list grows longer. Maybe we should stop treating ascites like a diet challenge and start treating it like a chronic disease with real people behind it.
Also, to the people who think ‘just eat less salt’ is the solution-you’ve never had to shop for groceries with a liver that can’t process anything. Try living on 2 grams of sodium when your only affordable protein is canned tuna packed in brine. Good luck.
So yeah. 2-3 grams. Let’s stop pretending we’re saving lives by making people miserable. We’re just making them compliant.
Also, vaptans cost $7k? Of course they do. Because capitalism.
And yes, I know this is a rant. But someone had to say it.
Jasper Arboladura
November 29, 2025 AT 18:17There’s a fundamental flaw in the premise of this article. The 2022 Gut and Liver study you cite has a selection bias-it excluded patients with severe hyponatremia, which is precisely the population most at risk from moderate sodium intake. The meta-analysis from Hepatology 2023, which included over 8,000 patients, showed a U-shaped curve: both ultra-low and moderate sodium intake increased mortality compared to mild restriction.
Also, the 45% resolution rate you cite doesn’t account for fluid reaccumulation within 30 days. That’s not resolution-it’s temporary compensation.
And the claim that strict sodium restriction causes hepatorenal syndrome? That’s backwards. HRS is caused by systemic vasodilation and renal hypoperfusion, not sodium restriction. In fact, sodium restriction reduces intravascular volume, which should theoretically *protect* renal perfusion by lowering portal pressure.
You’re conflating correlation with causation. Patients who can’t adhere to low-sodium diets are often sicker, more malnourished, and less compliant overall. Of course they do worse. It’s not the diet-it’s the disease progression.
And don’t get me started on the ‘personalized diet’ nonsense. Medicine isn’t Pinterest. We don’t ‘personalize’ evidence. We apply it. If the data says 2g is safe, then 2g is safe. If the patient can’t follow it, that’s a behavioral issue-not a protocol failure.
Also, albumin dosing at 8g/L? That’s outdated. The 2022 EASL guidelines recommend 6.25g/L for volumes under 5L, and 8g/L only for >5L. You’re citing a 2010 protocol.
Don’t mislead people with cherry-picked data and emotional appeals. This isn’t advocacy. It’s medical misinformation dressed as pragmatism.
Joanne Beriña
December 1, 2025 AT 09:38So let me get this straight-some fancy doctor in a lab coat is telling us to eat more salt because ‘it’s too hard’? Are you kidding me? This is America. We don’t bend to weakness. We don’t coddle patients with liver disease by giving them a free pass to eat processed junk.
If you can’t handle a 2-gram sodium limit, maybe you shouldn’t be alive. Your liver’s failing because you ate too much fried food and soda your whole life. Now you want to eat more salt because you’re too lazy to cook? That’s not medicine-that’s surrender.
And don’t even get me started on the ‘personalized diet’ nonsense. You think your grandma’s chicken noodle soup is ‘moderate’? That’s 1,200mg of sodium in one bowl. You’re not ‘personalizing’-you’re enabling.
Why are we letting people with cirrhosis get away with eating ramen, deli meat, and frozen pizza? This isn’t healthcare. It’s a buffet for bad choices.
And what about the cost? You want to give everyone albumin infusions? That’s taxpayer money funding poor decisions. If you can’t follow basic dietary rules, you don’t deserve a liver transplant.
Stop coddling. Start holding people accountable. That’s real medicine.
Also, if you’re on diuretics and still eating salt, you’re just wasting your doctor’s time. You’re not a patient. You’re a liability.
ABHISHEK NAHARIA
December 1, 2025 AT 15:48There is a profound epistemological disconnect between clinical guidelines and lived experience. The medical establishment, rooted in reductionist paradigms, continues to impose binary thresholds-2 grams, 3 grams-as if human physiology were a linear system governed by fixed coefficients.
Ascites is not merely a sodium problem. It is a systemic collapse of homeostatic regulation, wherein the kidney, liver, and vasculature are locked in a pathological feedback loop. To isolate sodium as the primary variable is to commit the fallacy of the single cause.
Moreover, the cultural context of dietary adherence is ignored. In India, for instance, the average sodium intake is 4.5 grams per day, primarily from fermented foods, pickles, and lentil-based dishes. To demand 2 grams is not medical advice-it is cultural erasure.
The PROMETHEUS trial is a step toward epistemic humility. But until we recognize that compliance is not a moral failing but a structural challenge-fueled by food deserts, poverty, and misinformation-we will continue to treat symptoms while ignoring the illness of the system.
Also, vaptans are not ‘expensive.’ They are commodified. The pharmaceutical industry does not innovate for health. It innovates for profit.
And let us not forget: the human body is not a machine. It does not respond to commands. It responds to meaning, to dignity, to trust. If we treat patients as problems to be fixed, we will never fix anything.
But of course, you already knew that.
Or did you?
Hardik Malhan
December 2, 2025 AT 20:26Portal hypertension drives ascites via RAAS overactivation and splanchnic vasodilation. Diuretics work by antagonizing aldosterone and inhibiting Na-K-2Cl cotransport. But sodium restriction alone doesn’t reduce portal pressure-it reduces intravascular volume, which can worsen renal perfusion if not titrated with albumin or volume expansion.
The 2-3g sodium target is physiologically sound because it balances natriuresis without triggering compensatory vasopressin release. Below 2g, you risk hyponatremia-induced cerebral edema and increased risk of HRS-AKI.
Spironolactone 100-400mg + furosemide 40-160mg is still first-line. Ratio should be 100:40. Higher ratios increase hypotension risk.
NSAIDs inhibit COX-2 in afferent arterioles → reduced GFR → worse ascites. ACEi/ARBs reduce efferent arteriolar tone → further GFR drop. Avoid.
Albumin dosing: 8g/L for >5L paracentesis. For <5L, 6g/L is sufficient per 2022 EASL.
Adherence is poor because food labeling is misleading. 75% sodium is hidden. Most patients don’t know what ‘low sodium’ means.
Personalization isn’t weakness. It’s precision medicine.
Also, vaptans: not for routine use. Only if hyponatremia and refractory ascites. And only if serum Na >125.
Monitoring: weight daily, Na weekly, creatinine twice weekly. If Na drops >5mEq/L in 48h, reduce diuretics.
Casey Nicole
December 4, 2025 AT 07:08so like… i just read this whole thing and i’m like… why is everyone so mad about salt? like i get it’s a thing but also… i have a friend with cirrhosis and she just eats what she wants and takes her meds and she’s doing fine? like maybe the real issue is we’re all so obsessed with control that we forget people are trying to survive not follow a textbook?
also the idea that you can just ‘cut salt’ when your only affordable food is canned soup and frozen dinners is laughable. i’m not saying eat junk but like… maybe the goal should be ‘don’t die’ not ‘eat like a monk’
and also who even has time to measure grams of sodium? i can’t even measure my coffee. my toddler eats more salt than i do and she’s 3.
also why is everyone acting like the liver is some kind of moral judge? it doesn’t care if you had fries or not. it just… stops working. and then you’re stuck.
so yeah. 2-3g sounds good. but also… just… don’t be a jerk to people who are already sick. they’re trying.
also i cried reading about the birthday cake. that’s not medicine. that’s cruelty.
Kelsey Worth
December 4, 2025 AT 16:27Okay but can we just talk about how the word ‘refractory’ sounds like a villain in a superhero movie? ‘The patient has developed refractory ascites… and now the world trembles.’
Also-why do we make patients feel guilty for wanting to taste their food? I’ve seen people cry because they couldn’t have a slice of pizza on their birthday. That’s not treatment. That’s emotional abuse wrapped in a white coat.
And the ‘2 grams’ thing? I’ve read the labels on ‘low sodium’ bread. It’s still 230mg per slice. That’s 920mg just from toast. You’re telling me someone’s supposed to eat one slice and then never have anything else salty again? That’s not a diet. That’s a prison.
Also, I love that we’re all pretending ‘moderate’ sodium is some radical new idea. My grandma had cirrhosis in the 90s and they just told her to ‘eat less salt’-not ‘eat zero salt.’
Maybe the real breakthrough isn’t in the guidelines. Maybe it’s in realizing that people aren’t problems to be solved. They’re people.
Also, I just googled ‘licorice root ascites’ and now I’m scared to eat candy again. Thanks, medicine.
shelly roche
December 6, 2025 AT 14:46Hey everyone-just wanted to say how much I appreciate this thoughtful discussion. It’s rare to see such a nuanced conversation about liver disease that actually includes the human side.
I work as a community health worker, and I’ve seen patients choose between paying for rent or buying low-sodium food. Some of them drive 40 miles to a specialty grocery store just to find bread without added salt. That’s not compliance-that’s devotion.
And you know what? They still show up to appointments. They still take their pills. They still try.
So when we talk about ‘non-adherence,’ let’s not forget: the system is failing them, not the other way around.
Also, I’ve seen patients get so much better on moderate sodium diets-because they’re actually eating real food, not just boiled chicken and lettuce. They’re getting protein. They’re getting calories. They’re getting joy.
And joy matters. It’s not fluffy. It’s physiological. Stress kills faster than sodium.
Let’s stop punishing people for being human.
And to the folks who say ‘if you can’t follow the diet, you don’t deserve care’-please. That’s not medicine. That’s cruelty disguised as discipline.
We can do better. We’re better than this.
And if you need help finding affordable low-sodium food in your area-I’ve got a list. DM me. I’ve got your back.
Nirmal Jaysval
December 7, 2025 AT 21:04Bro the whole thing is just fake science. In India we have cirrhosis from alcohol and hepatitis but we don’t even know what sodium is. We eat pickles, papad, and salted yogurt every day. Some of my cousins with liver disease are still alive and working. So why all this fuss?
Also diuretics make you pee all day. I know a guy who got dehydrated and passed out. Now he’s on dialysis. So maybe the real problem is doctors overtreating.
And vaptans? $7000? Are you kidding? In India we use cheap herbs and turmeric. Works fine.
Also why is everyone scared of salt? Salt is life. Without salt you die. The West is too scared of everything.
Just eat normal food. Take medicine. Don’t stress. Life is short.
Also I heard someone say ‘albumin’ like it’s magic. It’s just protein. Boil eggs. Eat dal. Done.
Stop overcomplicating. Simple is better.
Emily Rose
December 8, 2025 AT 12:22Can we just take a second to celebrate how far we’ve come? Ten years ago, patients with ascites were told to drink ‘no fluids’ and eat ‘zero salt.’ Now we’re having a real conversation about balance, quality of life, and individual needs.
That’s progress.
I’ve worked with patients who lost 10 pounds in a week on diuretics and ended up in the ER with kidney failure. We learned from that. We adjusted. We listened.
And now? We’re not just treating the liver-we’re treating the person.
Yes, sodium matters. But so does dignity. So does connection. So does the taste of a tomato.
Let’s keep pushing for guidelines that don’t just say ‘do this’ but ask ‘how can we help you do this?’
Also-thank you to everyone who shared their stories. You’re not just patients. You’re teachers.
And if you’re reading this and you’re scared or overwhelmed? You’re not alone. We’re in this together.
Benedict Dy
December 10, 2025 AT 00:41There is no ‘moderate sodium’ paradigm in evidence-based hepatology. The data is clear: sodium restriction below 2 g/day reduces mortality, hospitalization, and progression to HRS. The Gut and Liver study is an observational cohort with confounding by indication. Patients on higher sodium diets were younger, had better baseline renal function, and were more likely to be transplant candidates-none of which were adequately adjusted for.
Furthermore, the claim that ‘strict sodium restriction causes malnutrition’ is a red herring. Malnutrition in cirrhosis is due to anorexia, altered metabolism, and gut dysbiosis-not sodium restriction. In fact, low-sodium diets are often higher in vegetables, legumes, and lean protein-nutrient-dense foods that improve outcomes.
Albumin dosing at 8 g/L is correct per 2022 EASL for >5L paracentesis. The 6.25 g/L recommendation applies only to volumes under 5L and in the absence of circulatory dysfunction.
And let’s be unequivocal: vaptans are not cost-effective. They are not first-line. They are not recommended outside of clinical trials.
This article is not a balanced review. It is a polemic dressed as clinical guidance. It misrepresents the evidence. It undermines patient safety. And it is dangerous.
Do not deviate from established guidelines without prospective, randomized data.
And if you are a clinician reading this: your responsibility is to the evidence, not to the convenience of your patients.
Emily Nesbit
December 11, 2025 AT 00:42Correction: The 2022 Gut and Liver study did not find ‘better results’-it found a higher rate of initial fluid reduction, but no difference in 6-month survival or time to reaccumulation. The study’s primary endpoint was not clinically meaningful. Also, the ‘low-sodium’ group consumed 1.2g sodium/day-not 2g. That’s not ‘strict’-that’s pathological.
Also, the claim that ‘ultra-low sodium increases HRS risk’ is not supported by RCTs. The only RCT on this (SODIUM-HEP, 2021) found no difference in HRS incidence between 1.5g and 3g sodium groups.
Albumin dosing: 8g/L is correct for volumes >5L. But the study cited used 10g/L, which is excessive and increases volume overload risk.
NSAIDs: 2.3x risk of ESRD? That’s from a single retrospective cohort with poor adjustment for baseline kidney function. The OR drops to 1.4 after multivariate analysis.
This article is riddled with misinterpretations, cherry-picked data, and misleading statistics. It is not evidence-based. It is opinion masquerading as science.
And the ‘personalized diet’ narrative? That’s not medicine. That’s marketing.
Don’t confuse compassion with clinical negligence.
John Power
December 11, 2025 AT 17:09I just want to say thank you to everyone who shared their stories. This isn’t just about salt or diuretics-it’s about being seen.
I’m a nurse who’s been working with cirrhosis patients for 15 years. I’ve seen people lose their jobs because they couldn’t eat what everyone else ate. I’ve seen them skip meds because they couldn’t afford the follow-up labs. I’ve seen them hide their swelling because they didn’t want to be a burden.
And I’ve also seen them thrive-not because they followed every rule perfectly-but because someone listened to them.
So if you’re reading this and you’re scared, or tired, or guilty-please know this: your worth isn’t measured in grams of sodium.
It’s measured in how hard you fight. And you’re fighting.
And you’re not alone.
Also-if you need help finding low-cost food options or transportation to appointments-I’ve got resources. Just ask. No judgment. Just help.
Richard Elias
December 12, 2025 AT 06:56So let me get this straight-you’re telling me the answer to cirrhosis is… eat more salt? And you call that medicine? You’re not helping. You’re enabling. You’re giving people permission to die faster.
And you want to replace guidelines with ‘personalization’? That’s just code for ‘we don’t have the willpower to enforce standards.’
Also, ‘moderate sodium’? That’s what you call it when you can’t be bothered to educate your patients. That’s not a treatment plan. That’s surrender.
And the ‘birthday cake’ thing? Cute. But this isn’t a feel-good story. This is end-stage liver disease. People die from this. And you’re giving them permission to eat chips and soup and pretend it’s okay.
Stop romanticizing noncompliance. Stop calling it ‘quality of life.’ It’s just giving up.
And if you’re a doctor and you’re prescribing this… you should be ashamed.
Jordyn Holland
December 12, 2025 AT 21:22Wow. So the ‘evidence-based’ crowd just threw a temper tantrum because someone dared to say ‘people are real.’
Let me guess-you think malnutrition is ‘just a side effect’ and not a driver of mortality? You think a patient who eats 2000 calories a day of rice and lentils is ‘better off’ than one who eats 1800 calories of salmon and vegetables because the sodium is 0.2g higher?
And you call that ‘compassion’? That’s dogma with a lab coat.
Also, you say ‘no difference in survival’ in the Gut and Liver study? Then why did they need 60% fewer paracenteses? Why did their hospitalizations drop? Why did their quality of life scores improve?
Because sometimes, survival isn’t just about living longer. It’s about living with dignity.
And if you can’t see that, maybe you’re the one who needs to be treated.
Also, I’m not ‘enabling.’ I’m humanizing.
And you? You’re just scared of a world where medicine isn’t about control.
Good luck with that.
shelly roche
December 13, 2025 AT 08:30Thank you for saying that. I’ve had patients tell me they stopped taking their meds because they felt like monsters for eating a slice of pizza. That’s not treatment. That’s trauma.
And you know what? The ones who were allowed to have *something* they loved-just one thing-ended up more consistent with everything else. Their labs improved. Their mood lifted. They showed up.
It’s not about the sodium.
It’s about trust.
And trust? You don’t build it with guidelines. You build it with listening.
So yes. Let them have the cake.
And then help them get the care they need.
That’s medicine.
Not fear.
Not control.
Just care.