Drug Substitution: When Switching Meds Is Safe — and When It’s Not
When you hear drug substitution, the practice of replacing a prescribed medication with another that’s considered medically similar. Also known as generic substitution, it’s meant to save money — but it’s not always harmless. Many people assume a generic pill is just a cheaper version of the brand, and for most drugs, that’s true. But for some, even tiny differences in fillers, coatings, or release timing can change how your body responds — sometimes dangerously.
Take NTI drugs, narrow therapeutic index medications where small changes in blood levels can cause serious harm. Drugs like levothyroxine for thyroid function or warfarin for blood thinning fall into this group. A 10% shift in absorption might mean your thyroid stops working right, or your blood clots when it shouldn’t. That’s why many doctors and pharmacists avoid switching these unless absolutely necessary. Then there’s therapeutic equivalence, the official rating system that says two drugs are interchangeable. But that rating doesn’t always match real life. Two generics might both be labeled "therapeutically equivalent," but if one has a different coating that slows absorption, you could feel worse — even if the active ingredient is identical.
And it’s not just about generics. Sometimes, a doctor switches you from one brand to another brand, or from one class of drug to another, thinking they’re the same. But excipients, the inactive ingredients like dyes, fillers, or preservatives, can trigger allergies, digestive issues, or even affect how the drug is absorbed. One person might switch from brand to generic and feel fine. Another might get headaches, nausea, or mood swings — all because of a different starch or coating. These reactions are real, often ignored, and rarely reported.
What you’ll find below isn’t theory. It’s real stories from people who switched meds and got sick. It’s the hidden rules hospitals use when drug shortages hit. It’s the list of drugs where switching isn’t allowed — even if the pharmacy wants to. It’s how to spot when a substitution is risky, what questions to ask your pharmacist, and when to push back. You don’t need to be a doctor to protect yourself. You just need to know what to look for.
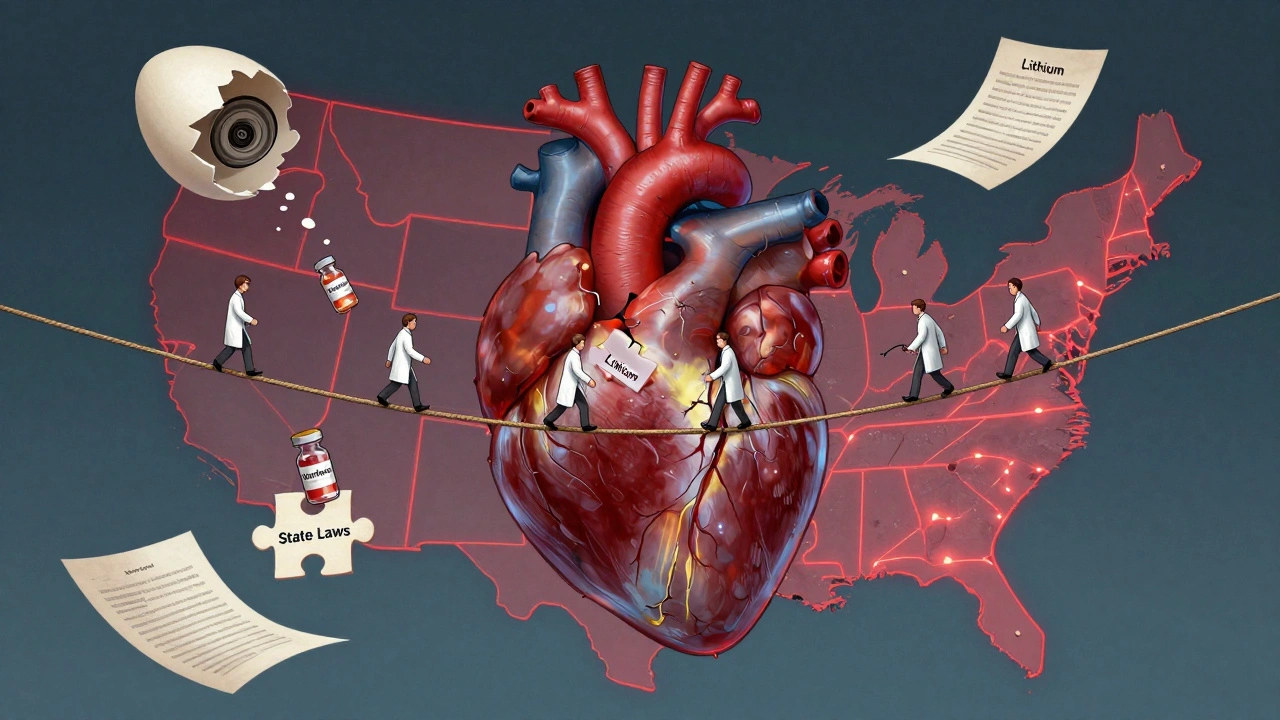
State Laws on NTI Drug Substitution: How Rules Differ Across the U.S.
State laws on NTI drug substitution vary widely across the U.S., with 27 states restricting generic swaps for medications like warfarin and levothyroxine due to safety risks. The FDA disagrees, but patient outcomes suggest restrictions matter.
About
Medications