Generic Drug Replacement: What You Need to Know Before Switching
When you hear generic drug replacement, a substitute medication with the same active ingredient as a brand-name drug, often at a lower cost. Also known as generic substitution, it's a routine part of modern pharmacy practice—but not all switches are created equal. Many people assume generics are just cheaper copies of the same thing. That’s mostly true—but what’s hidden in the fillers, coatings, and manufacturing process can make a real difference in how your body responds.
Here’s the thing: the active ingredient, the chemical that treats your condition, like levothyroxine or sildenafil in a generic must match the brand. But the excipients, the non-active ingredients like dyes, binders, and coatings that help the pill hold together or dissolve don’t have to. For most people, that’s fine. But if you’re sensitive to lactose, gluten, or certain dyes, a generic might trigger side effects your brand-name drug never did. That’s not a flaw in the generic—it’s a mismatch between your body and the formulation.
Some drugs, like NTI drugs—narrow therapeutic index medications such as warfarin or levothyroxine—require extreme precision. Even tiny changes in absorption can throw off your dose. Studies show patients on these drugs often do better staying on the same version, brand or generic, because switching can lead to unstable blood levels. That’s why many doctors and pharmacists recommend sticking with one version unless there’s a clear reason to change.
And it’s not just about safety. When you switch to a generic, you might not notice a difference right away—but over months or years, small variations in how your body absorbs the drug can add up. That’s why long-term health tracking matters. If you’ve been on a brand-name drug for years and feel stable, ask your doctor: is switching really necessary? Or is it just cost-saving pressure?
Not all generics are equal, either. The same drug made by different manufacturers can vary in how fast it dissolves or how consistently it releases into your system. That’s why the therapeutic equivalence, the official FDA rating that says two drugs are interchangeable matters. Look for the "AB" rating in the Orange Book—it means the generic has passed bioequivalence tests and is considered interchangeable. "B" rated? That’s a red flag. Don’t assume it’s safe to swap.
Drug shortages, insurance rules, and pharmacy substitutions make switching unavoidable sometimes. But you don’t have to accept it blindly. Know your options. Ask your pharmacist: "Is this generic rated AB?" "What’s the manufacturer?" "Has anyone else reported side effects with this version?" Keep a journal of how you feel after a switch. If your symptoms change—fatigue, dizziness, mood swings—don’t brush it off. It might not be your condition. It might be the filler.
Below, you’ll find real-world stories, clinical insights, and hard data on what happens when people switch to generics. Some stay healthy. Others face unexpected problems. We’ll show you how to spot the difference—and how to protect yourself no matter what your prescription says.
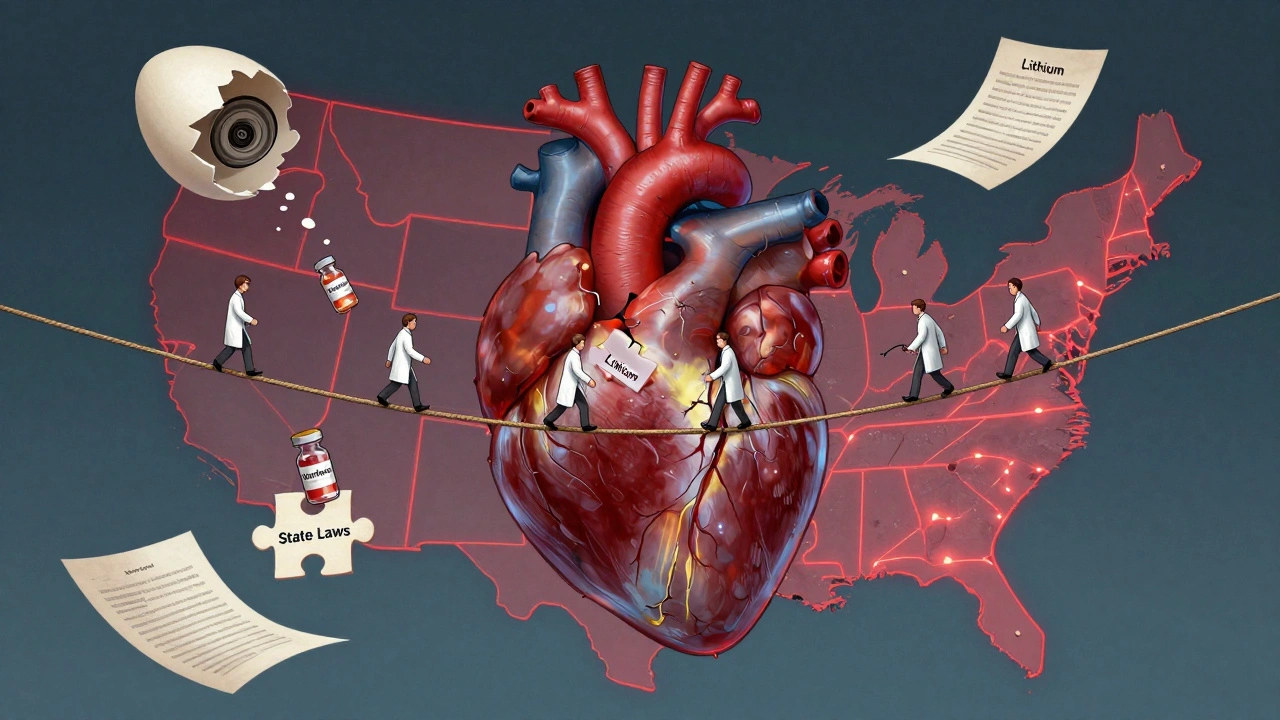
State Laws on NTI Drug Substitution: How Rules Differ Across the U.S.
State laws on NTI drug substitution vary widely across the U.S., with 27 states restricting generic swaps for medications like warfarin and levothyroxine due to safety risks. The FDA disagrees, but patient outcomes suggest restrictions matter.
About
Medications