NTI Drugs: What They Are, Why They Matter, and How to Use Them Safely
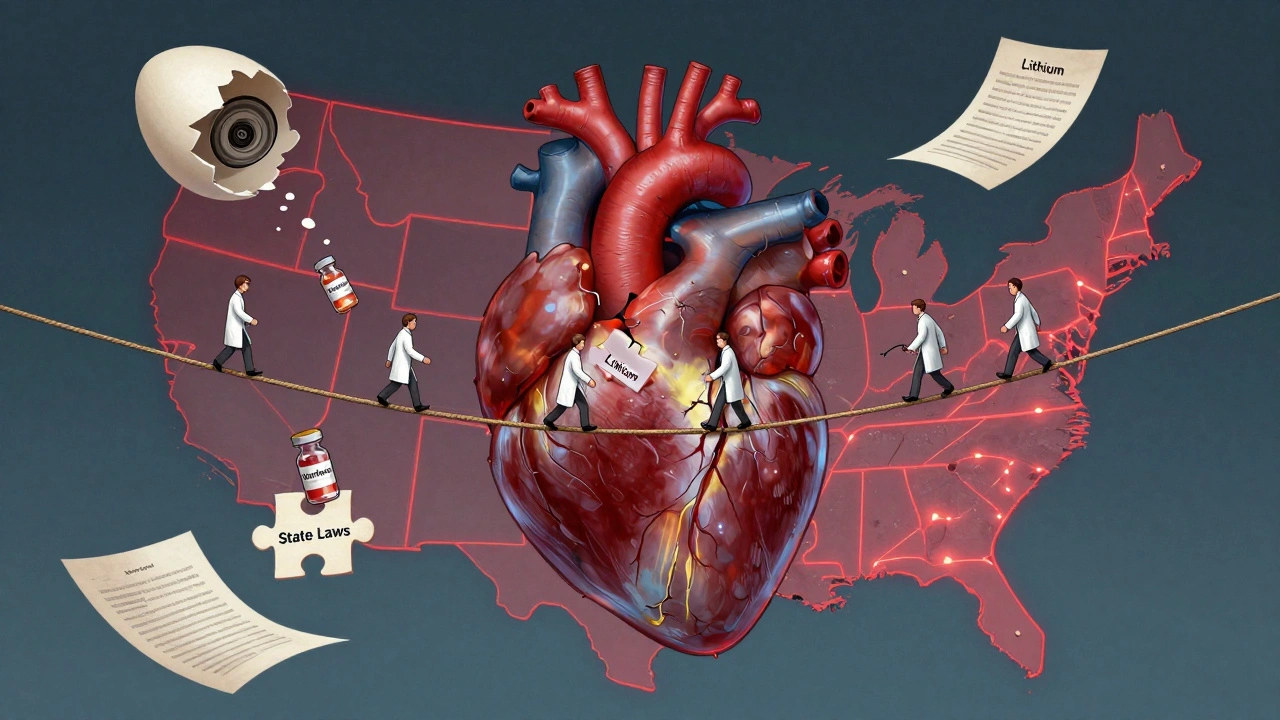
When a medication has a narrow therapeutic index, a range between the effective dose and the toxic dose so small that even minor changes can lead to harm or treatment failure. Also known as NTI drugs, these are not your typical prescriptions—they demand precision. Think of them like a tightrope walk: one step too far, and things go wrong fast. Drugs like warfarin, levothyroxine, phenytoin, and cyclosporine fall into this category. They work well when dosed just right, but too little won’t help, and too much can land you in the hospital.
That’s why generic substitution, the practice of swapping a brand-name drug for a cheaper generic version. Also known as generic switching, it gets risky with NTI drugs. Even if two pills have the same active ingredient, differences in fillers, coatings, or how fast they dissolve can push your blood levels out of the safe zone. A 2019 study in the Journal of the American Pharmacists Association found that patients on warfarin who switched generics had a 20% higher chance of abnormal blood clotting or bleeding within 30 days. That’s not a small risk—it’s a red flag.
This is where therapeutic equivalence, the idea that two drugs perform the same way in the body. Also known as bioequivalence, it gets messy. The FDA says generics are equivalent—but for NTI drugs, "equivalent" doesn’t always mean "safe to swap." Many doctors and pharmacists avoid switching these unless absolutely necessary. Even then, they monitor blood levels closely. If you’re on one of these drugs, don’t assume your pharmacist’s substitution is harmless. Ask: "Is this safe for my specific NTI medication?" and "Will I need a blood test after the switch?"
You’ll also see these topics come up in posts about drug safety, how side effects from excipients can surprise you, and why some people react differently to generics even when the active ingredient is identical. These aren’t theoretical concerns—they’re real, documented cases. Someone on levothyroxine who switches brands and suddenly feels exhausted? That’s not "just stress." It’s a dose that’s now too low. Someone on phenytoin who starts having seizures after a generic switch? That’s not bad luck—it’s a narrow therapeutic window they didn’t know they were walking.
What you’ll find in the posts below aren’t just general guides on generics or drug interactions. They’re focused, practical breakdowns of how these exact issues play out in real life: how dose differences in combination drugs matter, why some people can’t tolerate generics even when they’re "approved," and how health systems manage these risks when drug shortages hit. This isn’t about theory. It’s about keeping you safe when your medicine leaves no room for error.
State Laws on NTI Drug Substitution: How Rules Differ Across the U.S.
State laws on NTI drug substitution vary widely across the U.S., with 27 states restricting generic swaps for medications like warfarin and levothyroxine due to safety risks. The FDA disagrees, but patient outcomes suggest restrictions matter.
About
Medications