State Pharmacy Laws: What You Need to Know About Prescription Rules and Regulations
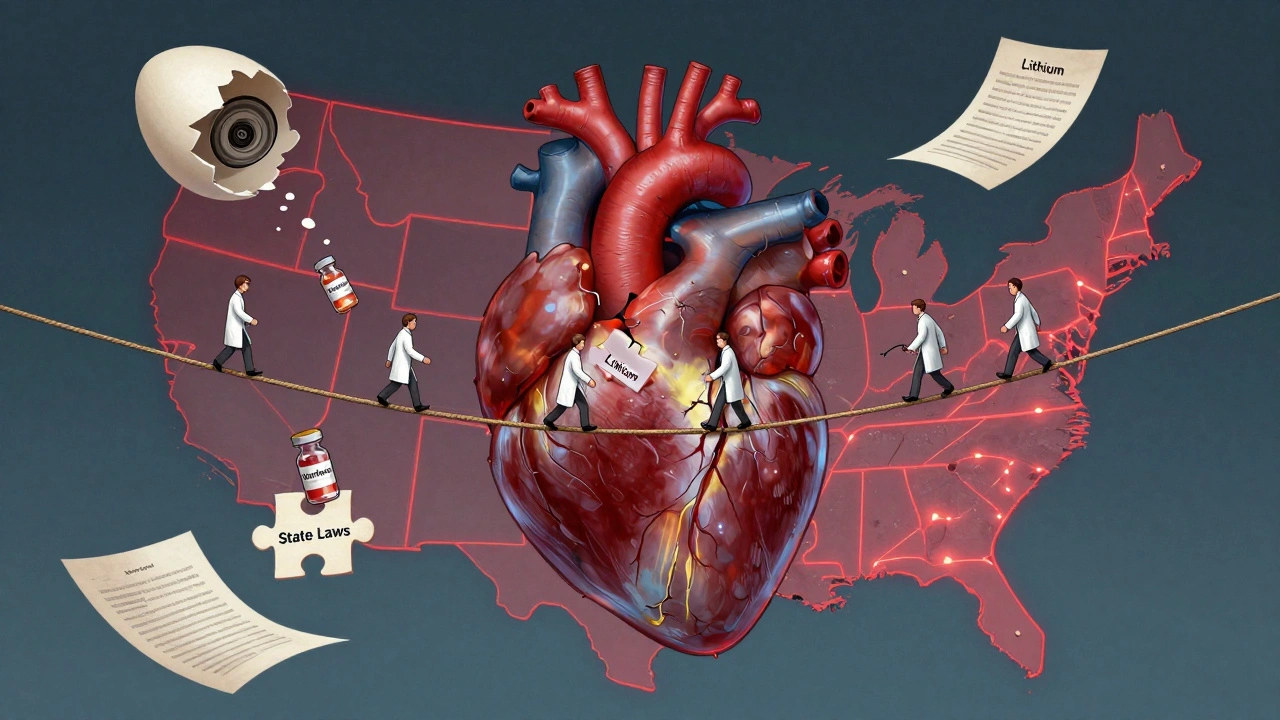
When you pick up a prescription at the pharmacy, you’re not just dealing with a pharmacist—you’re navigating a complex web of state pharmacy laws, legally enforced rules that govern how medications are dispensed, stored, and tracked within each U.S. state. Also known as pharmacy regulations, these rules are set by each state’s board of pharmacy and can differ dramatically from one location to another. What’s allowed in California might be illegal in Texas, and a drug you can buy over the counter in one state could require a prescription in another.
These laws cover everything from pharmacist licensing, the certification and ongoing requirements for pharmacists to practice legally in a state, to how controlled substances, drugs like opioids, benzodiazepines, and stimulants that have high potential for abuse are tracked through prescription monitoring programs. Some states require pharmacists to check a state database before filling any opioid prescription. Others mandate that pharmacies store certain drugs behind the counter or limit the quantity you can buy in a single visit. Even something as simple as refilling a prescription without a new doctor’s note can be restricted—or required—depending on where you live.
State pharmacy laws also shape how pharmacies handle generic substitutions, telepharmacy, and even who can administer vaccines. In some states, pharmacists can prescribe certain medications under collaborative agreements with doctors. In others, they’re strictly limited to dispensing what’s written on the script. These differences directly impact your access to care, your out-of-pocket costs, and even your safety—especially when switching pharmacies or moving between states.
The posts below dig into real-world issues tied to these rules: why generic substitution isn’t always safe for certain drugs like levothyroxine, how drug shortages force pharmacies to make tough choices, and what happens when pharmacy policies clash with patient needs. You’ll find practical advice on navigating prescription refills, understanding why some meds require extra paperwork, and how to protect yourself when state rules don’t match federal guidelines. Whether you’re a patient, caregiver, or healthcare worker, knowing how these laws work in your area isn’t just helpful—it’s essential.
State Laws on NTI Drug Substitution: How Rules Differ Across the U.S.
State laws on NTI drug substitution vary widely across the U.S., with 27 states restricting generic swaps for medications like warfarin and levothyroxine due to safety risks. The FDA disagrees, but patient outcomes suggest restrictions matter.
About
Medications