Statin Types: Which Ones Work Best and What You Need to Know
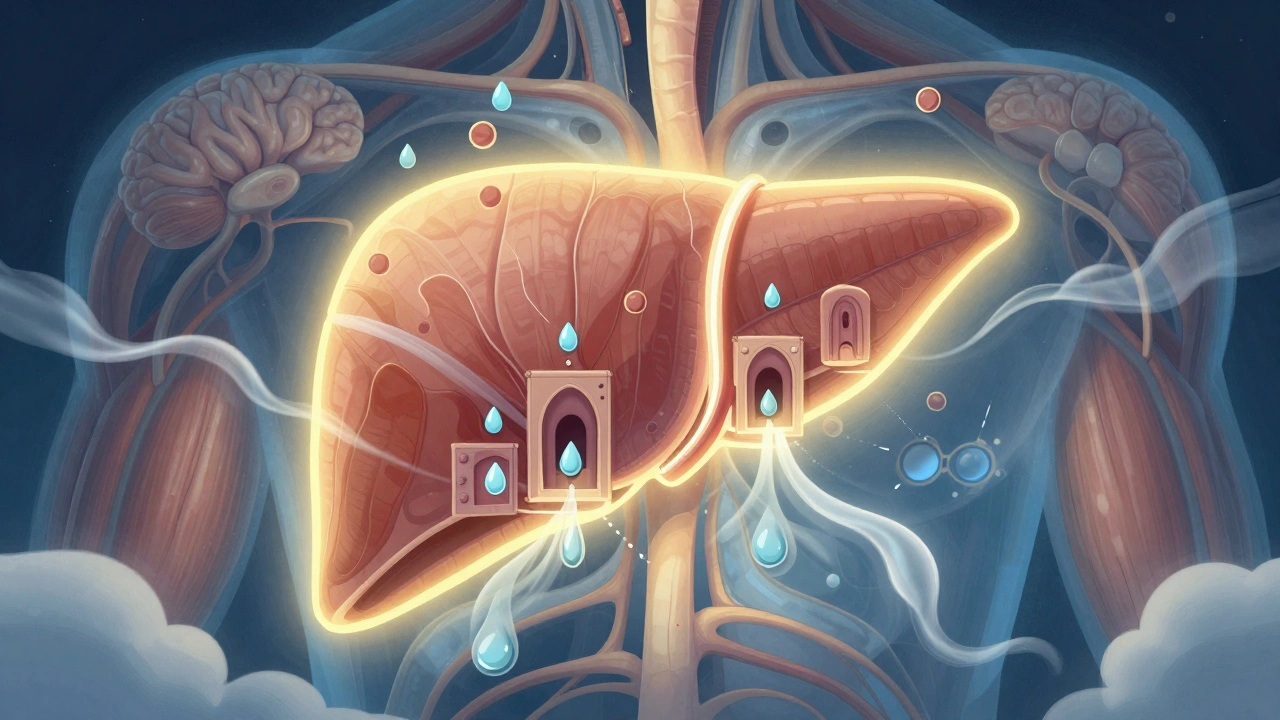
When your doctor talks about statin types, a class of drugs used to lower cholesterol by blocking a liver enzyme that makes LDL, or "bad" cholesterol. Also known as HMG-CoA reductase inhibitors, they’re among the most prescribed medications in the world because they cut heart attack risk by up to 30% in high-risk patients. But not all statins are created equal. Some are stronger, some last longer, and some cause more side effects—like muscle pain or liver stress—depending on your body and other meds you take.
The big five statin types you’ll hear about are atorvastatin, a long-acting statin often used for high cholesterol and heart disease prevention, rosuvastatin, the most potent at lowering LDL, sometimes called the "super statin", simvastatin, a cheaper option that works well for many but has more drug interactions, pravastatin, a gentler statin often chosen for older adults or those with liver concerns, and fluvastatin, a weaker statin sometimes used when others cause side effects. Each one has a different strength, how long it stays in your system, and how it’s processed by your liver. For example, atorvastatin and rosuvastatin are taken once daily and aren’t as affected by food, while simvastatin works better at night and can interact badly with grapefruit or certain antibiotics.
What’s often overlooked is that generic versions of these statins work just as well as brand names—like Lipitor or Crestor—but cost a fraction. Many people switch to generics without issues, but some notice side effects from the fillers or coatings, not the active drug. If you’ve had muscle aches or fatigue after switching, it’s not always the statin itself—it could be the inactive ingredients. That’s why some patients stick with brand, even when generics are available. And if you’re on other meds, like blood thinners or diabetes drugs, your statin choice matters even more. Some statins interfere with how those drugs are broken down, which can lead to dangerous buildup in your system.
There’s no one-size-fits-all statin. Your age, liver health, other conditions, and even your diet play a role. What works for your neighbor might not work for you. The posts below dig into real patient experiences, how doctors pick the right statin type, what side effects to watch for, and how to talk to your provider about switching or adjusting your dose. You’ll find practical advice on managing muscle pain, understanding blood tests, and avoiding dangerous interactions—all based on actual pharmacy and clinical insights.
Hydrophilic vs Lipophilic Statins: What You Need to Know About Side Effects
Understanding the difference between hydrophilic and lipophilic statins helps explain why some people experience muscle pain or other side effects. Not all statins work the same way, and your best choice depends on your health, age, and other meds.
About
Medications