Every time you take a pill, you're making a bet. The drug might help you feel better, but it could also hurt you - sometimes in ways no one saw coming. This isn't fear-mongering. It's science. Medication safety isn't just about reading the label or asking your pharmacist. It's about understanding the hidden math behind every prescription: the balance between what a drug can do for you, what it might do to you, and how we actually know which one is more likely.
Why Clinical Trials Don't Tell the Whole Story
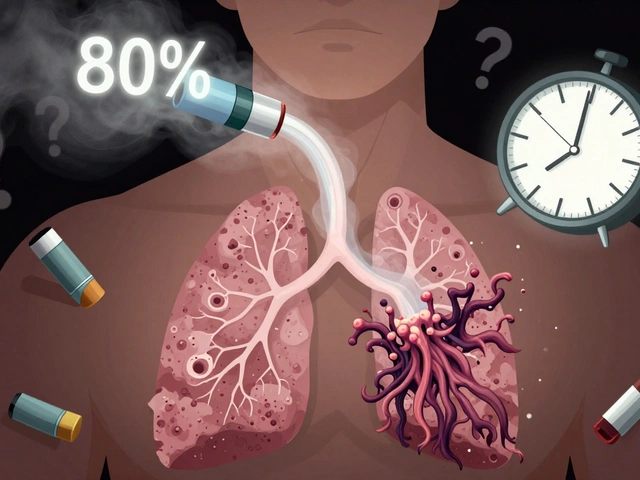
Think about how drugs get approved. A company runs a trial with maybe 2,000 people over a year or two. That sounds like a lot - until you realize that in the real world, millions of people take the same drug, often for years, sometimes with other medications, sometimes with chronic conditions the trial didn't include. That's where things go off-script. A rare side effect that shows up in 1 out of 10,000 people won't show up in a trial of 5,000. That’s basic math. But when that drug hits the market and 500,000 people start taking it, suddenly you’ve got 50 cases of something no one predicted. That’s how we learned about the heart risks of some painkillers, the suicidal thoughts linked to certain antidepressants in young adults, or the dangerous drop in blood pressure from mixing common drugs. That’s why the real work of medication safety doesn’t start when a drug is approved - it starts right after. This is where pharmacoepidemiology comes in. It’s the science of studying how drugs behave in real populations, not just in controlled labs. It’s the bridge between what a drug does in a trial and what it does when Grandma takes it with her blood pressure pills, her arthritis cream, and her daily aspirin.How We Track What Drugs Really Do
Researchers don’t guess. They dig. And they use big data like never before. The FDA’s Sentinel Initiative tracks health records from over 190 million Americans. Kaiser Permanente’s system holds data on 12.5 million patients. Medicare claims cover 57 million seniors. These aren’t just numbers - they’re millions of real stories, each one a clue. There are three main ways they look for trouble:- Cohort studies: Follow a group of people who took a drug and compare them to those who didn’t. Did more people in the drug group have a stroke? That’s a red flag.
- Case-control studies: Find people who had a bad reaction, then look back to see what they were taking. Compare them to people who didn’t have the reaction.
- Self-controlled designs: Smart trick. Look at one person over time. Did they have a problem only when they were on the drug? That cuts out a lot of noise - like age, lifestyle, or other illnesses.
The Trade-Off Between Proof and Practicality
Randomized controlled trials (RCTs) are still the gold standard. They’re the reason we know statins lower heart attack risk. But they’re slow and expensive - often costing $26 million and taking years. And they’re designed to answer one question: “Does this drug work under ideal conditions?” Real life isn’t ideal. People forget pills. They mix drugs. They have kidney problems or liver disease. That’s where observational studies shine. They cost maybe $300,000 - a fraction of an RCT - and can answer questions like: “Does this drug cause kidney damage in people over 70 who also take diuretics?” Here’s the catch: 22% of the strong links found in observational studies were later disproven by RCTs. That’s not a failure - it’s a reminder that science is messy. The goal isn’t perfection. It’s progress. We use RCTs to approve drugs. We use real-world data to watch them after they’re out there. The FDA now requires risk evaluation and mitigation strategies (REMS) for high-risk drugs. That means companies must monitor side effects closely, train doctors, and sometimes restrict who can get the drug. It’s not perfect, but it’s a system built on evidence - not guesswork.
Where Things Go Wrong in Real Life
Even with all the science, mistakes still happen - and they often come from the front lines. Nurses report near-miss errors weekly because EHR systems are fragmented. One doctor orders a drug. Another doesn’t see it. A pharmacist flags a warning. The doctor overrides it because they’ve seen it 100 times before. That’s alert fatigue. One study found prescribers ignore 89% of drug interaction alerts - especially for common meds. Older adults are especially vulnerable. Fifteen percent of Medicare patients have a preventable adverse drug event every year. Why? Because they’re on five or more medications. That’s not rare. It’s normal. And each new pill adds another chance for conflict. Opioids are another crisis. In 2022, 80,000 people in the U.S. died from opioid overdoses. That’s not just addiction - it’s a failure of safety systems. Doctors didn’t know how fast dependence could happen. Patients didn’t know the risks. The evidence was there - but it wasn’t acted on quickly enough. At Kaiser Permanente, they fixed one problem by creating a simple protocol for alcohol withdrawal. Instead of guessing doses, they used a standardized plan. Severe withdrawal cases dropped by 42%. That’s not magic. That’s science applied.What’s Changing Now - And What’s Next
The field is moving fast. In 2023, the FDA launched Sentinel System 3.0 - a real-time monitoring tool that can flag safety signals in days, not years. AI is being tested to predict who’s most at risk for an adverse event before it happens. Early results show a 22-35% drop in high-alert medication errors. Soon, wearables could feed data into safety systems. Heart rate spikes, sleep patterns, activity levels - all of it might help spot early signs of a bad reaction. Imagine knowing your blood pressure dropped because of a new drug before you even felt dizzy. But there are risks. A 2023 Supreme Court decision weakened some privacy protections for health data used in research. And compounded drugs - mixed in pharmacies, not made by big labs - are largely unmonitored. The GAO flagged this as a major gap in 2024. The future isn’t about replacing doctors or trials. It’s about building smarter systems. Drug companies are investing heavily - the global pharmacovigilance market is expected to hit $11.7 billion by 2028. Hospitals with over 300 beds now have dedicated medication safety officers. That’s a good sign. But smaller clinics? Only 28% do. That’s where the next wave of improvement needs to hit.
What You Can Do
You don’t need to be a scientist to protect yourself. Here’s what actually works:- Keep a list: Write down every pill, supplement, and cream you take. Bring it to every appointment. Even the “harmless” ones.
- Ask questions: “What’s this for?” “What if I miss a dose?” “Could this interact with my other meds?” Don’t be shy. Doctors expect it.
- Know your risk: If you’re over 65, on five or more drugs, or have kidney or liver problems, you’re at higher risk. That doesn’t mean avoid meds - it means be extra careful.
- Report side effects: If something feels off - even if it seems small - tell your doctor. And report it to the FDA’s MedWatch program. One report won’t change anything. Ten thousand might.
How do I know if a medication is safe for me?
There’s no single answer, but you can reduce risk. First, tell your doctor and pharmacist every medication, supplement, and herb you take - including over-the-counter ones. Ask if the new drug interacts with anything you’re already on. Check if you’re in a high-risk group - like being over 65 or having kidney or liver disease. Use a pill organizer and stick to the schedule. If something feels wrong, don’t ignore it. Report it.
Are generic drugs as safe as brand-name ones?
Yes. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand-name drug. They must also meet the same strict manufacturing standards. The only differences are in inactive ingredients - like fillers or dyes - which rarely cause problems. If you’ve had a reaction to a brand-name drug, ask your pharmacist if the generic has the same inactive ingredients.
Why do drug warnings keep changing after a medication is approved?
Because safety isn’t proven in a lab - it’s discovered in the real world. Clinical trials involve a few thousand people for a short time. Once millions start using the drug, rare side effects appear. New interactions show up. Long-term risks emerge. That’s why the FDA updates labels - sometimes adding black box warnings, sometimes restricting use. It’s not a failure. It’s how the system is supposed to work.
Can AI really help prevent medication errors?
Yes - and it already is. Hospitals using AI-driven systems to predict which patients are most likely to have an adverse drug event have seen 22-35% fewer errors with high-risk medications. These tools analyze your medical history, current meds, lab results, and even your age and weight to flag potential risks before a prescription is filled. But they’re not foolproof. Human oversight is still essential.
What’s the biggest threat to medication safety today?
Polypharmacy - taking five or more medications daily - is the biggest silent threat. It’s especially common in older adults. Each additional drug increases the chance of harmful interactions, side effects, and dosing errors. The problem isn’t the drugs themselves - it’s the lack of coordinated care. When multiple doctors prescribe without seeing the full picture, the risk skyrockets. Regular medication reviews with one provider can cut this risk significantly.




Chad Kennedy
December 2, 2025 AT 17:41This post is way too long... I just want to know if my pill is gonna kill me or not. Why do they make it sound like a PhD thesis? Ugh.
Siddharth Notani
December 3, 2025 AT 07:08Respected author, your exposition on pharmacovigilance is both meticulous and illuminating. The integration of real-world evidence with clinical frameworks represents a paradigm shift in patient safety. One must acknowledge the systemic rigor underpinning such initiatives as Sentinel and REMS. A commendable contribution to public health discourse.
Cyndy Gregoria
December 4, 2025 AT 21:13You’re not alone. I’m 71 and on six meds. I keep a list on my phone and show it to every doc. It’s scary how easy it is for things to slip through. But you CAN protect yourself - start small. Write down one thing today. You’ve got this.
Akash Sharma
December 6, 2025 AT 09:31Actually, this is fascinating because it highlights a fundamental tension in medical science - the gap between controlled environments and the messy reality of human biology. Clinical trials are designed to eliminate confounders, sure, but that also means they exclude the very people who need the drug most - elderly patients with comorbidities, pregnant women, those on polypharmacy regimens. And yet, we prescribe to them anyway. The observational studies you mention aren’t just ‘backup’ data - they’re the only data that truly matters for real patients. I’ve been reading about the self-controlled case series method and it’s brilliant - using each person as their own control removes so much noise from demographic and lifestyle variables. But here’s the kicker: most primary care docs don’t even know these methods exist. They see a black box warning and panic, or worse, ignore it because ‘it’s always been fine.’ The real bottleneck isn’t the science - it’s the translation. How do we get this info to the bedside without overwhelming clinicians? Maybe AI-driven alerts are the answer, but only if they’re smart enough to prioritize - not just bombard. And what about the 22% of observational findings that get debunked by RCTs? That’s not noise - it’s the scientific process. We’re learning. We’re adapting. But the system moves slower than the data. And that’s the tragedy.
Palanivelu Sivanathan
December 7, 2025 AT 02:19Broooooo… this isn’t just about pills… it’s about TRUST. Who are we trusting? The FDA? The pharma giants? The doctor who’s rushing between 30 patients? We’re all just guinea pigs in a giant, silent experiment - and the worst part? We’re PAYING for it. 😭💊 The system is broken. We’re told ‘trust science’… but science is just a word used by people with white coats to sell you hope. And now they want us to trust AI? Ha! AI doesn’t care if you die. It just crunches numbers. What happened to human judgment? What happened to the art of medicine? I feel like we’re all just… data points. In a machine. That’s not progress. That’s dehumanization. 😔
Joanne Rencher
December 8, 2025 AT 21:36Of course the FDA updates warnings - because they’re lazy and let companies push drugs through without proper long-term studies. And now we’re supposed to ‘report side effects’? Like that does anything. I reported my panic attacks from Zoloft. Nothing happened. They don’t care. You’re just a number. Don’t be fooled by the ‘science’ talk. It’s all PR.
Cristy Magdalena
December 9, 2025 AT 10:43There’s a disturbing lack of accountability here. The system isn’t ‘messy’ - it’s negligent. If a drug causes 50 deaths among 500,000 users, that’s not ‘basic math’ - that’s a preventable catastrophe. And yet, the FDA approves it anyway. And then we’re told to ‘be informed’? As if a patient can parse epidemiological studies before filling a prescription. This isn’t empowerment - it’s victim-blaming. The burden of safety is placed on the most vulnerable, while corporations profit and regulators shrug. The fact that 89% of drug interaction alerts are ignored? That’s not ‘alert fatigue’ - that’s a design failure. Someone should be fired. Someone should be sued. But no - we just keep taking pills and hoping for the best. Pathetic.
Adrianna Alfano
December 9, 2025 AT 11:57my grandma took 8 meds and one time she got super dizzy and i thought it was just old age but it was the new blood pressure pill mixing with her diuretic. we found out because i kept asking questions. now she has a med review every 3 months. i’m not a nurse but i learned how to read a med sheet. if you’re over 65, PLEASE do this. even if your doctor says ‘it’s fine’ - ask again. i cried when i saw how many interactions were flagged. no one ever told us. we just trusted. and that’s the problem. we trusted too much. but we can change it. one list. one question. one report. it matters. 🙏