Antidepressant Tapering Calculator
Stopping antidepressants safely requires careful planning. The right tapering schedule depends on your medication type, duration of use, and individual factors. This tool provides general guidelines to help you discuss a safe plan with your healthcare provider.
Recommended Tapering Duration
Based on your medication type and duration of use, we recommend a tapering period of:
This is a general guideline - your doctor may adjust based on your specific situation.
Key Considerations
- Start with the smallest possible dose reduction (e.g., 10-25% of your current dose)
- Wait at least 2-4 weeks between each dose reduction
- Track your symptoms using a journal or symptom tracker
- Consider switching to fluoxetine (Prozac) as a buffer for faster-acting antidepressants
Stopping antidepressants isn’t as simple as just skipping a pill. For many people, it triggers a cascade of physical and mental symptoms that feel terrifyingly real - dizziness, electric shock sensations in the head, nausea, insomnia, and a sense of being detached from reality. These aren’t signs of relapse. They’re not weakness. They’re antidepressant discontinuation syndrome, a well-documented physical withdrawal reaction that affects up to 80% of people who stop abruptly after taking these drugs for more than a month.
What Exactly Is Antidepressant Discontinuation Syndrome?
Antidepressant discontinuation syndrome happens when your body has adapted to the presence of the medication and suddenly loses it. This isn’t addiction in the way people think of drugs like opioids or benzodiazepines. You don’t crave the drug. You don’t use it to get high. But your brain has rewired itself to function with the drug’s presence. When it’s gone, your neurotransmitters - especially serotonin and norepinephrine - go into temporary chaos.
The term was originally pushed by pharmaceutical companies to downplay the idea that antidepressants cause dependence. But medical evidence now confirms this is a real, physiological withdrawal. The American Academy of Family Physicians recognized it back in 2006, and since then, research has only strengthened that view. It’s not a myth. It’s not "all in your head." It’s your nervous system recalibrating.
The Symptoms: More Than Just Feeling Off
Symptoms vary, but they often follow a pattern. Doctors use the mnemonic FINISH to remember the most common signs:
- Flu-like symptoms: Fatigue, muscle aches, chills, headaches, diarrhea
- Insomnia: Trouble falling or staying asleep, vivid or disturbing dreams
- Nausea: Feeling sick to your stomach, sometimes vomiting
- Ibalance: Dizziness, vertigo, unsteady walking
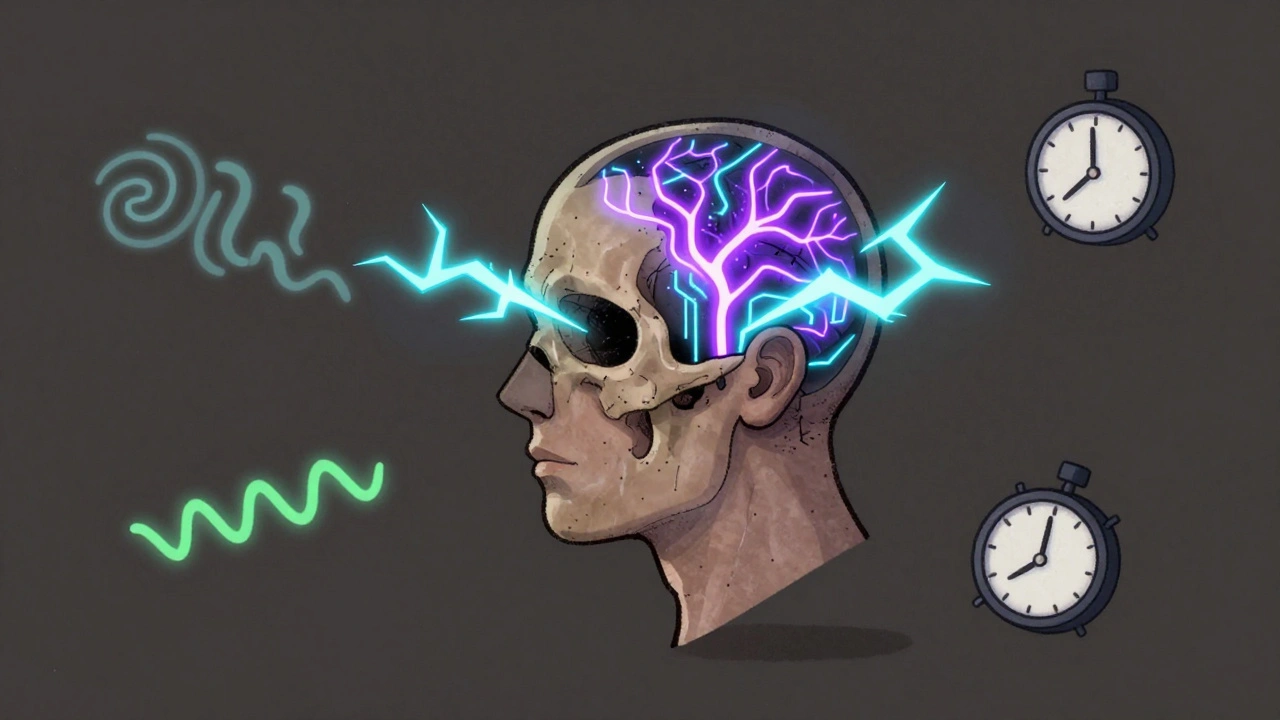
- Sensory disturbances: "Brain zaps" - sudden, brief electric shock feelings, especially when moving your eyes
- Hyperarousal: Anxiety, irritability, agitation, panic attacks
Some people report feeling like there’s "cotton wool" in their head, trouble concentrating, or even derealization - the sense that the world around them isn’t real. Others experience anger outbursts, mood swings, or akathisia - that unbearable inner restlessness where you can’t sit still.
These symptoms don’t show up right away. For most, they start within 2 to 4 days after the last dose. But if you’re taking a drug with a short half-life - like paroxetine or venlafaxine - they can hit within hours of missing a pill. That’s why some people wake up feeling awful after forgetting their morning dose.
Not All Antidepressants Are the Same
The risk and severity of withdrawal depend heavily on the type of antidepressant you’re taking.
SSRIs like sertraline, escitalopram, and fluoxetine are the most commonly prescribed. Paroxetine, despite being an SSRI, is notorious for causing severe withdrawal because it leaves your system quickly. Fluoxetine, on the other hand, sticks around for days - so its withdrawal is usually milder and slower.
SNRIs like venlafaxine and duloxetine often cause worse symptoms than SSRIs. One study found nearly half of people stopping venlafaxine experienced significant withdrawal. The combination of serotonin and norepinephrine disruption hits harder.
TCAs - older drugs like amitriptyline - can cause movement issues: tremors, stiff muscles, balance problems that mimic Parkinson’s. These are often overlooked.
MAOIs are the most dangerous to quit cold turkey. Symptoms can include severe agitation, confusion, hallucinations, and even catatonia. Stopping these without medical supervision can be life-threatening.
It’s Not Relapse - But It’s Hard to Tell the Difference
This is where things get confusing. Many people think their return of sadness or anxiety means their depression is coming back. But there’s a key difference.
Relapse takes time. If your original depression symptoms return, they usually build slowly over weeks. Discontinuation symptoms hit fast - within days. And they’re different. You won’t just feel sad. You’ll feel physically unwell: dizzy, nauseous, zapping with electric shocks.
Worse, some symptoms - like low mood or anxiety - overlap. That’s why up to 38% of cases get misdiagnosed. Someone goes to their doctor with dizziness and panic attacks after stopping sertraline, and they’re told, "It’s your depression returning," so they’re put back on the same drug - not because they need it, but because the doctor didn’t recognize withdrawal.
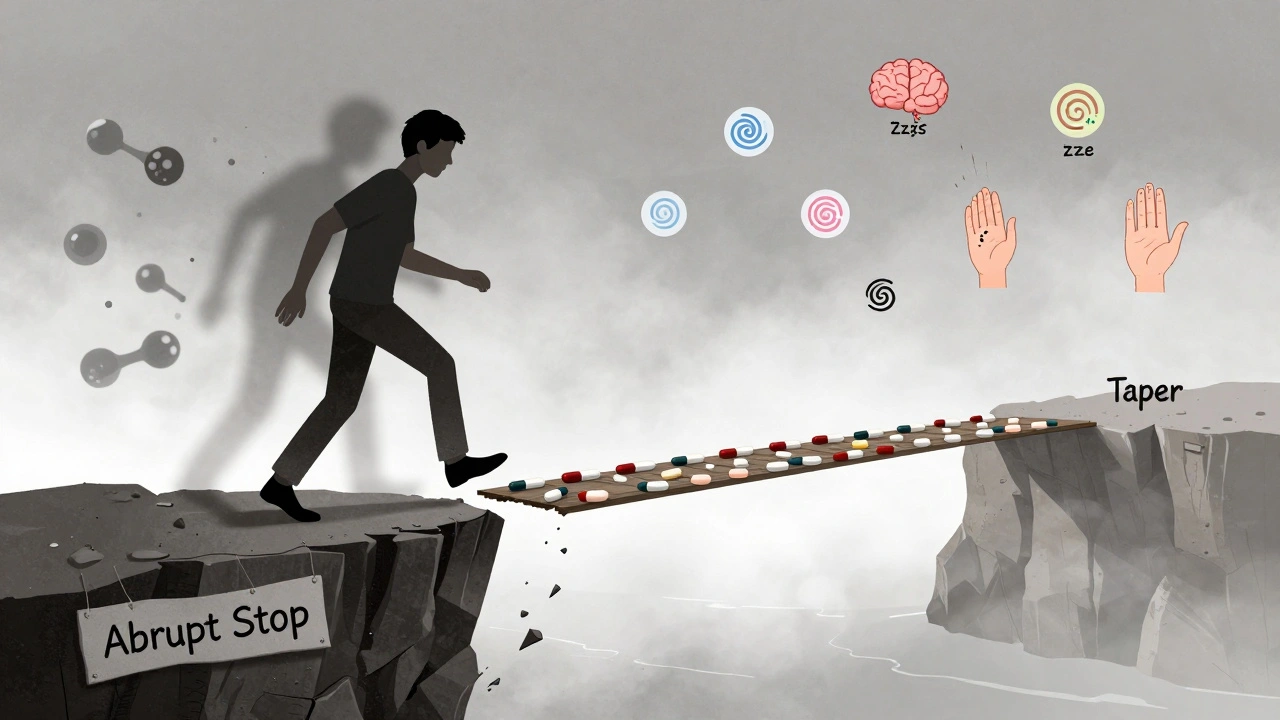
How to Avoid It: Tapering Is Everything
The best way to avoid discontinuation syndrome? Don’t stop abruptly. Ever.
Doctors recommend tapering - slowly reducing your dose over time. For most SSRIs, that means at least 4 to 6 weeks. For SNRIs like venlafaxine, 8 weeks or more is safer. The longer you’ve been on the drug, the slower you should go.
Some people need even longer. If you’ve been on antidepressants for years, a 3- to 6-month taper might be necessary. There’s no one-size-fits-all schedule. Your doctor should personalize it based on your medication, how long you’ve taken it, and your individual sensitivity.
Switching between brands or generics can also trigger symptoms. Not all formulations are bioequivalent. A switch from one generic version to another might lower your blood levels enough to cause withdrawal - even if you didn’t change the dose.
And if you’re pregnant? About 4 in 10 women stop their antidepressants without medical advice during pregnancy. That’s risky. Withdrawal can be dangerous for both mother and baby. Always talk to your doctor before making any changes.
What If You Already Stopped and Feel Terrible?
If you’ve already stopped and are experiencing symptoms, don’t panic. You’re not alone. And it’s not permanent.
The fastest fix? Reintroduce the original medication. Most people feel better within 72 hours. That’s a clear sign it’s withdrawal - not relapse. If you feel better after taking your usual dose, then slowly taper again under supervision.
If you can’t restart the same drug - maybe you had side effects or your doctor wants you to switch - switching to fluoxetine can help. Because fluoxetine has such a long half-life, it acts like a buffer. Your body gets a slow, gentle reduction instead of a sudden drop.
Some people use liquid formulations or pill cutters to make smaller reductions. Others use compounding pharmacies to create custom low-dose capsules. These aren’t available everywhere, but they’re options worth discussing with your prescriber.

Protracted Withdrawal: When Symptoms Last for Months
Most medical guides say withdrawal lasts 1 to 2 weeks. That’s true for many. But it’s not the full story.
Community data from Surviving Antidepressants - a peer support group with over 15,000 members - shows that 73% of people report symptoms lasting longer than two weeks. Nearly 30% say they’ve struggled for six months or more. Brain zaps, fatigue, brain fog, and emotional sensitivity can linger.
Recent studies back this up. A 2022 paper in the Journal of Clinical Psychiatry found nearly 19% of people had symptoms lasting over three months. This isn’t rare. It’s underreported.
Why? Because doctors aren’t trained to expect it. Patients are told, "It’ll pass in a week." When it doesn’t, they feel broken. They think they’re failing. They’re not. This is a physiological response that takes time to heal - sometimes longer than we’ve been taught.
What You Can Do Right Now
If you’re thinking about stopping:
- Don’t do it alone. Talk to your prescriber - even if you think you’re fine.
- Ask about your medication’s half-life. Short half-life? Prepare for a slower taper.
- Request a tapering plan in writing. Know the schedule before you start.
- Track your symptoms. Note when they start, how bad they are, and what helps.
- If you feel awful after missing a dose - don’t ignore it. Contact your doctor immediately.
If you’re already in withdrawal:
- Don’t blame yourself. This isn’t weakness.
- Reach out to support groups. You’re not the only one.
- Ask about fluoxetine bridging if you can’t restart your original drug.
- Be patient. Healing takes time. Rest, hydration, and gentle movement help more than you think.
Final Thoughts
Antidepressants save lives. But they’re not harmless. Stopping them without care can cause real, distressing symptoms - and too many people are left confused and alone when they happen.
The medical community is slowly catching up. Guidelines are changing. More doctors are learning to recognize withdrawal. But patients still bear the burden of being the first to speak up.
If you’re on antidepressants and considering stopping - don’t rush. Ask questions. Demand a plan. And if you’ve already stopped and feel off - know that you’re not crazy. You’re experiencing a real, documented reaction. And help is available.
Can antidepressants cause physical dependence?
Yes. While antidepressants aren’t addictive in the way drugs like opioids are, they can cause physical dependence. Your body adapts to their presence, and stopping suddenly leads to withdrawal symptoms. This is called antidepressant discontinuation syndrome. It’s not about craving or misuse - it’s about your nervous system needing time to readjust.
How long do antidepressant withdrawal symptoms last?
Most people feel better within 1 to 2 weeks after tapering. But for some, symptoms can last months. Studies show nearly 1 in 5 people have symptoms beyond three months, and a significant number report issues lasting six months or longer. This is called protracted withdrawal, and while it’s less common, it’s real and increasingly recognized.
Are brain zaps dangerous?
Brain zaps - sudden electric shock-like sensations in the head - are not dangerous, but they can be very unsettling. They’re a hallmark of SSRI and SNRI withdrawal and are linked to changes in brain signaling. They usually fade over time. If they’re severe or accompanied by seizures, confusion, or loss of consciousness, seek medical help immediately - but those are extremely rare.
Can I switch to a different antidepressant to avoid withdrawal?
Sometimes. Switching to fluoxetine (Prozac), which has a very long half-life, can help smooth the transition. This is called a "bridge" strategy. But switching antidepressants isn’t always safe or effective. It should only be done under medical supervision, because it can cause new side effects or even worsen symptoms.
Is it safe to stop antidepressants during pregnancy?
Stopping antidepressants during pregnancy without medical guidance is risky. About 41% of pregnant women stop their medication on their own, but this can trigger withdrawal symptoms that affect both mother and baby. Untreated depression also carries risks. The best approach is to work with a psychiatrist and OB-GYN to weigh the risks and develop a safe plan - which may include tapering slowly or switching to a safer medication.




Rupa DasGupta
December 5, 2025 AT 07:26Marvin Gordon
December 5, 2025 AT 21:51ashlie perry
December 6, 2025 AT 04:43Juliet Morgan
December 6, 2025 AT 11:40Norene Fulwiler
December 7, 2025 AT 07:25William Chin
December 8, 2025 AT 18:26Katie Allan
December 10, 2025 AT 07:33Deborah Jacobs
December 11, 2025 AT 20:01James Moore
December 12, 2025 AT 05:34