Many people take benzodiazepines for anxiety or sleep, but few realize how deeply these drugs can affect the brain - and how hard it is to stop. If you’ve been on them for months or years, you might notice things aren’t quite right: forgetting where you put your keys, feeling unsteady on your feet, or struggling to focus. These aren’t just side effects - they’re warning signs backed by decades of research. And if you’re thinking about quitting, you need to know the right way to do it - because stopping cold can be dangerous.
How Benzodiazepines Hurt Memory
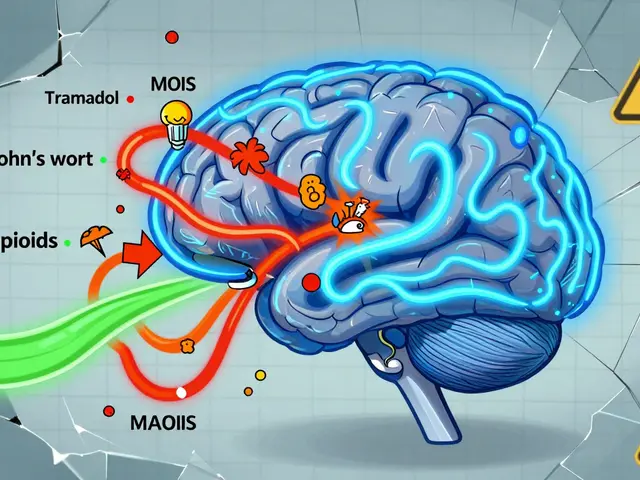
Benzodiazepines don’t just make you drowsy. They interfere with how your brain forms new memories. This isn’t about forgetting your birthday - it’s about not remembering what you had for breakfast, or why you walked into a room. That’s called anterograde amnesia, and it’s built into how these drugs work. They boost GABA, the brain’s main calming chemical, but in doing so, they slow down the hippocampus - the area responsible for turning short-term experiences into lasting memories. Studies from the 1980s still hold up today: even a single dose of diazepam or lorazepam can make it harder to remember new information. The worse the task, the bigger the drop in performance. Trying to learn a new phone number? You’re likely to forget it in minutes. Following a complex conversation? You’ll zone out. And here’s the kicker: these memory problems get worse the longer you take the drug. A 2023 review of 19 studies found that long-term users showed clear declines in recent memory, processing speed, and attention. On average, their cognitive scores dropped as much as someone with early-stage dementia. That’s not a metaphor - it’s what the data shows. IQ scores fell by 10 to 15 points. Reaction times slowed by 15% to 25%. Even after stopping, nearly half of users still struggled with memory and focus months later. One study tracking people for 10 months after quitting found only 45% returned to normal brain function.Why Falls Are a Silent Crisis
If you’re over 65 and taking a benzodiazepine, you’re at a 50% higher risk of falling. That’s not a small number. It’s the difference between a minor stumble and a broken hip - which can end your independence for good. These drugs don’t just make you sleepy. They blur your sense of balance, slow your reflexes, and make your muscles feel heavy. A 2014 analysis of over a million people showed benzodiazepine users were 70% more likely to suffer a hip fracture. It’s not just about old age. Even younger adults on these drugs have worse coordination. One study found a 30% drop in balance control after just one dose. Imagine trying to step off a curb or get up from the toilet in the middle of the night - your body just doesn’t react fast enough. That’s why the American Geriatrics Society has listed benzodiazepines as inappropriate for older adults since 2012. They’re not just risky - they’re often unnecessary. In the U.S. alone, benzodiazepines lead to over 93,000 emergency room visits for falls each year. And the risk isn’t the same for every drug. High-potency ones like alprazolam and lorazepam are twice as dangerous as older, longer-acting ones like diazepam. But no matter which one you take, the danger is real.
The Tapering Truth: Why Slow Is Safe
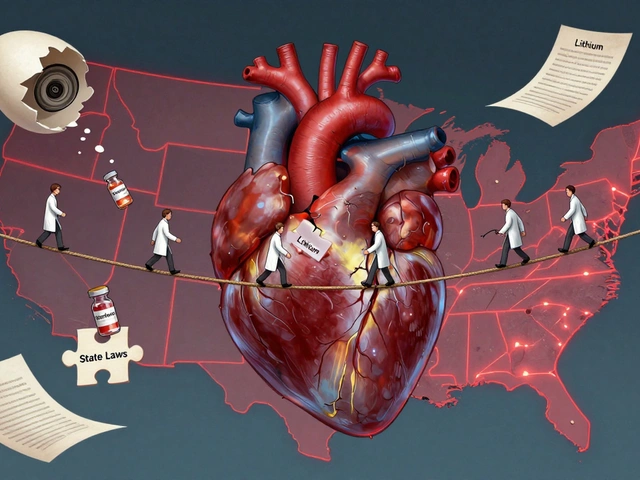
Quitting benzodiazepines isn’t like stopping a painkiller. Your brain adapts. It changes how its receptors work to compensate for the drug. When you remove it, your nervous system goes into overdrive. Rebound anxiety, insomnia, panic attacks, even seizures - these aren’t just possible. They’re common if you quit too fast. The gold standard for tapering is the Ashton Protocol. Developed in the 1980s by Professor C. Heather Ashton, it’s still the most trusted method today. The rule? Reduce your dose by 5% to 10% every one to two weeks. For long-term users, even slower is better - sometimes as little as 2% to 5% per month. The goal isn’t speed. It’s stability. A 2021 trial with 312 people showed that switching from a short-acting benzodiazepine to diazepam (which leaves the body slowly) and tapering over 12 to 16 weeks led to a 68.5% success rate at six months. Compare that to just 27% in the group that didn’t taper properly. The people who succeeded didn’t just stop the drug - they got their brain back. By week eight, many reported better focus, faster thinking, and clearer memory. But it’s not easy. About 22% needed to pause their taper for a few weeks because symptoms flared up. Eight percent couldn’t continue at all. That’s why having a doctor who understands this process matters. Self-tapering without support often ends in relapse - or worse.
What Recovery Looks Like
People who stick with a slow taper often report a slow but real return of mental clarity. It doesn’t happen overnight. Many describe it as “lifting a fog.” Brain fog, memory lapses, trouble concentrating - these don’t vanish the day you stop. But over six to twelve months, most see steady improvement. One survey of over 1,200 people who tried to quit found that 73% of those who tapered slowly reported better cognition after a year. The key? Patience. Users on forums like Reddit’s r/benzowithdrawal swear by tools like BrainBaseline to track daily changes. They also recommend using diazepam for tapering - not because it’s better for anxiety, but because its long half-life makes withdrawal smoother. There’s also good news on the horizon. New drugs are being tested that target only specific GABA receptors - the ones that calm anxiety without touching memory. Early results show these experimental drugs reduce anxiety just as well as traditional benzodiazepines - but without the brain fog. They’re not available yet, but they prove the damage isn’t inevitable.When to Talk to Your Doctor
If you’ve been on benzodiazepines for more than four weeks, you should have a conversation about stopping. The American Psychiatric Association says they shouldn’t be used long-term for anxiety. Yet millions are still prescribed them for months or years. Ask for a cognitive screen. The MoCA or MMSE test takes 10 minutes and can show if your memory or attention is already affected. If your score drops by 2 to 3 points over six months, it’s a red flag. Your doctor should consider discontinuing the drug - not just reducing the dose. And if you’re thinking about quitting, don’t do it alone. Find a provider who knows the Ashton Protocol. Ask about switching to diazepam first. Ask about support groups. Ask what your cognitive scores were before you started. That baseline matters. There’s no shame in needing help. What’s dangerous is staying silent because you think it’s normal to feel foggy, tired, or unsteady. It’s not. And you don’t have to live that way forever.Can benzodiazepines cause permanent brain damage?
No, benzodiazepines don’t cause permanent structural brain damage. Brain scans of long-term users show no shrinkage or lesions. But they do cause lasting functional changes - meaning your brain’s wiring and chemistry get stuck in a slowed-down state. That’s why memory and focus problems can linger for months after stopping. The good news? Most people see significant improvement over 6 to 12 months with a proper taper.
Is it safe to quit benzodiazepines cold turkey?
No. Stopping suddenly can trigger severe withdrawal, including seizures, hallucinations, and extreme anxiety. Even people who’ve taken low doses for a few months can have dangerous reactions. Always taper under medical supervision. The Ashton Protocol is the safest approach.
Why is diazepam used for tapering instead of other benzodiazepines?
Diazepam has a long half-life - it stays in your system for days. This means withdrawal symptoms build up slowly, giving your brain time to adjust. Short-acting drugs like alprazolam or lorazepam wear off quickly, causing sharp spikes in anxiety and insomnia between doses. Switching to diazepam smooths the process.
How long does it take to recover cognitively after stopping?
Improvement starts within 4 to 8 weeks for many, but full recovery often takes 6 to 12 months. Processing speed and attention tend to bounce back first. Memory and executive function take longer. Some people report ongoing mild issues after a year, but the majority see major gains. Tracking progress with simple memory or focus tests helps stay motivated.
Are there alternatives to benzodiazepines for anxiety and sleep?
Yes. For anxiety, SSRIs like sertraline or escitalopram are first-line treatments with no risk of dependence. For sleep, cognitive behavioral therapy for insomnia (CBT-I) is more effective long-term than any sleep pill. Melatonin, magnesium, or low-dose trazodone may help in some cases. Always discuss options with your doctor - there are safer paths.


Jason Stafford
January 3, 2026 AT 12:37The pharmaceutical industry is deliberately keeping these drugs on the market because they’re profitable. The FDA? Complicit. Doctors? Paid off. You think this is about patient care? No - it’s about control. Benzodiazepines aren’t just drugs; they’re chemical mind-slowing agents designed to keep the population docile. Look at the numbers: 93,000 ER visits from falls? That’s not an accident. That’s systemic suppression. They don’t want you awake. They don’t want you thinking. And they sure as hell don’t want you quitting.
They’ll tell you to ‘taper slowly’ - but who wrote that protocol? A pharma-funded researcher. The Ashton Protocol? A distraction. Real recovery means going off everything - cold turkey - with raw willpower. No diazepam swaps. No ‘support groups.’ Just you, your nervous system, and the truth they buried.
I’ve seen it. My cousin was on lorazepam for 8 years. They told her to taper. She quit cold. Seizures? Yes. Hallucinations? Yes. But after 14 months? She’s lucid. She remembers her daughter’s birthday. She drives again. They lied to her for a decade. Don’t let them lie to you.
This isn’t medicine. It’s chemical enslavement. And the clock is ticking.
jigisha Patel
January 4, 2026 AT 15:21While the post cites several studies, it fails to account for heterogeneity in patient populations. The 2023 meta-analysis referenced included patients with comorbid psychiatric conditions, which independently contribute to cognitive decline. The 10–15 point IQ drop is misleading - it conflates state-dependent impairment with trait-level deficits. Moreover, the Ashton Protocol’s 68.5% success rate assumes strict adherence, which is unrealistic in real-world settings where 40% of patients discontinue before week 12.
Furthermore, the comparison to early-stage dementia is hyperbolic. Dementia involves neurodegeneration; benzodiazepine-induced impairment is pharmacodynamic and reversible. The post ignores dose-response relationships - low-dose, short-term users show negligible cognitive impact. And let’s not forget: for many, these drugs are life-saving. A bipolar patient on 0.5mg clonazepam nightly isn’t ‘foggy’ - they’re functional. Pathologizing all use ignores clinical nuance.
Rory Corrigan
January 4, 2026 AT 19:11It’s funny how we treat the brain like a machine you can just reboot…
We’ve been conditioned to believe that consciousness is something you can optimize - like a smartphone. Take a pill, fix the anxiety. Take another pill, fix the sleep. And when it breaks? We blame the pill, not the system that made us need it in the first place.
The real tragedy isn’t the memory loss - it’s that we’ve forgotten how to sit with discomfort. How to breathe through panic without chemical anesthesia. How to be human without a pharmacological crutch.
The Ashton Protocol isn’t a cure. It’s a ritual. A slow unwinding of dependency - not just on drugs, but on the idea that we need to be fixed.
Maybe the fog isn’t the enemy. Maybe it’s the space where we start to remember who we were before we started trying to fix ourselves.
Just saying.
Connor Hale
January 5, 2026 AT 21:31I’ve been off benzos for 18 months now. Took me 11 months to taper - diazepam, 2% every 3 weeks. It was brutal. Sleepless nights. Waves of dread that felt like drowning.
But here’s what no one tells you: the fog doesn’t lift all at once. It’s like waking up in a room you haven’t seen in years. First, you notice the light is different. Then you remember the smell of the carpet. Then you realize you can think in full sentences again.
I used to forget my wife’s name for 3 seconds. Now I remember her laugh. That’s worth every night of shaking.
Don’t rush it. Don’t compare your week 3 to someone else’s month 6. Recovery isn’t linear. But it’s real.
And yes - I still have bad days. But now I know they’re temporary. Before? I thought they were permanent. That was the worst part.
Catherine HARDY
January 7, 2026 AT 19:35Did you know that the CDC quietly stopped tracking benzodiazepine-related deaths in 2018? Why? Because the numbers were too high. And the VA? They’ve been quietly replacing benzos with antipsychotics for veterans - which are even more dangerous. They don’t want you to know that the same institutions telling you to ‘taper slowly’ are also the ones prescribing them in the first place.
And don’t get me started on insurance companies. They won’t cover CBT-I for insomnia… but they’ll pay for a 30-day supply of alprazolam any day. Why? Because pills are cheaper than therapy. And control is cheaper than freedom.
They’re not trying to help you. They’re trying to keep you dependent. And the Ashton Protocol? Just another way to make you feel like you’re doing something - while they keep the profits rolling in.
melissa cucic
January 8, 2026 AT 00:27While the article presents compelling evidence regarding cognitive decline and fall risk, it is essential to contextualize these findings within the broader framework of clinical psychiatry. Benzodiazepines remain a vital therapeutic tool for acute anxiety, status epilepticus, and alcohol withdrawal - conditions where the risk-benefit ratio is unequivocally favorable.
Moreover, the assertion that long-term use leads to dementia-level cognitive deficits is overstated. Longitudinal studies (e.g., the Canadian Study of Health and Aging) show no causal link between benzodiazepine use and neurodegeneration. Functional impairment is reversible; structural damage is not - and the latter has not been demonstrated.
Furthermore, the Ashton Protocol, while widely cited, lacks robust randomized controlled trial validation beyond small cohorts. The 68.5% success rate cited derives from a single-center, non-blinded trial with significant selection bias.
It is irresponsible to generalize these findings to all users. For many, these medications enable functionality, not dysfunction. The goal should be individualized, patient-centered discontinuation - not blanket demonization.
Clint Moser
January 8, 2026 AT 09:18the ashton protocol is a joke. they want you to switch to diazepam? lmao. diazepam is just a longer-acting version of the same poison. you're still on a benzo. you're just slow-cooking your brain instead of microwaving it.
and the '68.5% success rate'? what's success? not having seizures? cool. but what about the 30% who still can't focus after a year? the ones who forget their kid's school play? the ones who feel like a ghost in their own body?
they say 'taper slow' - but they don't say how many people relapse because they can't handle the anxiety. they don't say that 70% of people who quit go back on within 2 years because the world is still f***ed and they're still broken.
the real answer? don't start. because once you're in, you're never really out.
Roshan Aryal
January 9, 2026 AT 14:04Western medicine is obsessed with pills. In India, we have yoga, pranayama, ayurveda - natural ways to calm the mind. Why are we importing American pharmaceuticals that turn brains to mush? This isn’t science - it’s cultural colonization.
My uncle took diazepam for 12 years. He forgot his own wedding anniversary. Then he quit - cold turkey, no doctor - and started drinking neem tea and doing kapalbhati every morning. Now he remembers every name, every date, every story from his childhood.
Why? Because the body heals when you stop poisoning it - and start living.
Stop trusting Big Pharma. Start trusting your ancestors.
Joseph Snow
January 9, 2026 AT 20:03This post is a classic example of medical fearmongering. The data is cherry-picked. The risks are exaggerated. The alternatives are oversimplified.
SSRIs? They cause sexual dysfunction, emotional blunting, and weight gain - and take 6–8 weeks to work. CBT-I? Only accessible to the wealthy or those with insurance. Melatonin? A placebo with a label.
Benzodiazepines are not perfect - but they are effective. For someone with severe panic disorder, a 0.5mg dose of lorazepam isn’t a cognitive killer - it’s a lifeline.
And let’s not pretend tapering is easy. The withdrawal symptoms are brutal. The relapse rate is astronomical. The post reads like a pamphlet from a cult that believes all pharmaceuticals are evil.
Real medicine doesn’t shame patients. It helps them survive.
Enrique González
January 11, 2026 AT 03:20I was on 2mg of lorazepam daily for 5 years. I couldn’t hold a conversation without zoning out. I’d walk into rooms and forget why.
I started tapering last year. Took 14 months. Used diazepam. Had a few setbacks. Cried a lot. Felt like I was losing my mind.
Now? I’m running 5Ks. I read books again. I remember dreams. I had a conversation with my mom yesterday - and actually remembered what she said.
It’s not glamorous. It’s not fast. But it’s worth it.
You’re not broken. You’re just medicated. And you can come back.
Siobhan Goggin
January 13, 2026 AT 00:56I’m so glad this post exists. I was terrified to quit - thought I’d never feel normal again. But I did. It took 10 months. I cried every week. But I’m here. And I’m proud.
If you’re reading this and you’re still on them - you’re not weak. You’re not broken. You’re just tired.
And you don’t have to live like this forever.
One day at a time.
Shanna Sung
January 14, 2026 AT 07:56They told me it was safe. They told me I could quit anytime. Then I tried. I had seizures. I lost 3 months of my life. They didn’t warn me. They didn’t care. Now I’m on disability. My kids don’t recognize me. And the doctors? They just shrug.
Don’t trust them. They don’t know what they’re doing. This is a war - and we’re the collateral damage.
Ashley Viñas
January 14, 2026 AT 18:46It’s heartbreaking to see how many people are suffering in silence - and how few doctors are trained to help them properly. I’ve worked in psych for 18 years. I’ve seen too many patients prescribed benzos for ‘stress’ - then stuck on them for decades.
The real tragedy isn’t the drugs. It’s the lack of alternatives. No one offers therapy. No one teaches breathwork. No one says: ‘Let’s try something else first.’
It’s easier to write a script.
And now we’re paying the price - with memory, with balance, with dignity.
But there’s hope. There really is.
Start slow. Find a good doctor. Be kind to yourself.
You’re not alone.
Justin Lowans
January 16, 2026 AT 05:42After reading this, I went back to my old journal from 2019. I was on 1mg of clonazepam. I wrote: ‘I don’t feel like me anymore.’
It took me 3 years to quit. I tapered with diazepam. I cried every week. I thought I’d never get my focus back.
Now? I write poetry again. I remember song lyrics. I laugh without feeling guilty.
It wasn’t the drug that broke me.
It was the silence.
Thank you for speaking up.