When you're taking an SSRI antidepressant like sertraline, escitalopram, or fluoxetine, you might assume it's safe as long as you don't miss a dose. But what you don't know could be dangerous. SSRI antidepressants are among the most commonly prescribed drugs in the U.S., with over 276 million prescriptions filled in 2022 alone. Yet, many people don’t realize that combining them with other medications-even common ones like painkillers or herbal supplements-can trigger serotonin syndrome, a potentially deadly condition.
What Is Serotonin Syndrome?
Serotonin syndrome isn’t just a side effect. It’s a medical emergency. It happens when too much serotonin builds up in your nervous system. This isn’t about feeling a little more anxious or jittery. This is about your body going into overdrive: muscles locking up, your temperature spiking past 104°F, uncontrollable shaking, confusion, rapid heartbeat, and sometimes seizures. The symptoms don’t come out of nowhere. They usually show up within hours of adding a new drug. One Reddit user described it after mixing sertraline with tramadol: "Within 12 hours, I couldn’t move my legs. I was sweating like I’d run a marathon in a sauna. The ER said I had serotonin syndrome. I spent three days in the hospital." Doctors use the Hunter Criteria to diagnose it-not vague feelings, but clear signs: spontaneous muscle spasms, clonus (involuntary twitching) with fever or sweating, or rigid muscles with high temperature and eye twitching. If you have one of these, it’s not a guess. It’s a diagnosis.Which Drugs Raise the Risk?
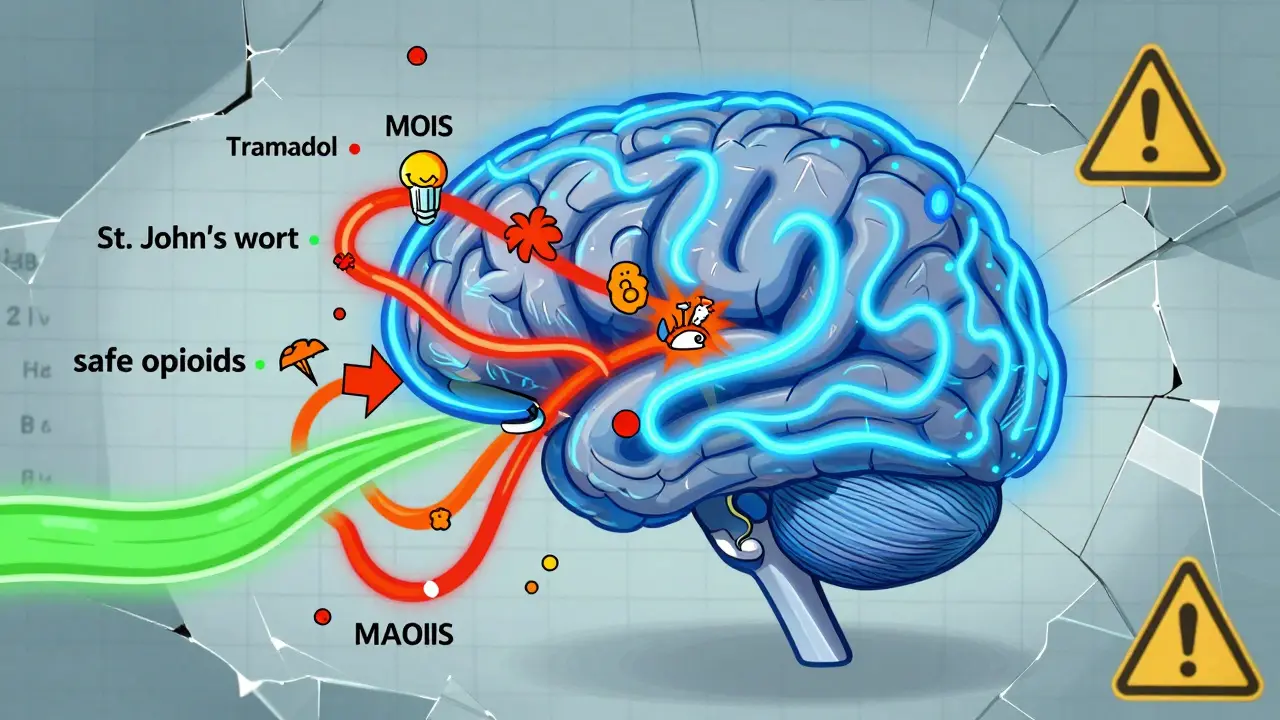
Not all drug combinations are equal. Some are harmless. Others are ticking time bombs. High-risk combinations:- SSRIs + MAOIs (like phenelzine or selegiline)
- SSRIs + linezolid (an antibiotic for resistant infections)
- SSRIs + tramadol, pethidine, or dextromethorphan (common pain and cough meds)
- SSRIs + methadone or fentanyl
- SSRIs + morphine, codeine, oxycodone, or buprenorphine
What About Herbal Supplements?
"Natural" doesn’t mean safe. St. John’s wort, a popular herbal remedy for mild depression, is a potent serotonin booster. One user on Drugs.com wrote: "I took St. John’s wort with my Prozac for three days. Then I started shaking so bad I couldn’t hold my coffee. The ER doctor said I was lucky I didn’t have a seizure." The FDA issued a black box warning in 2006 about this exact combo. Yet, many people still believe herbal supplements are harmless. They’re not. The same goes for tryptophan, 5-HTP, and even some energy drinks with high doses of L-tryptophan.
Why Are Some SSRIs Riskier Than Others?
Not all SSRIs are created equal. Their chemical makeup affects how long they stay in your body and how strongly they block serotonin reuptake.- Paroxetine has the strongest serotonin reuptake inhibition-95% according to a 2021 study. That means even small interactions can push you over the edge.
- Fluoxetine lasts the longest. Its active metabolite, norfluoxetine, sticks around for up to 15 days. If you stop fluoxetine and switch to an MAOI, you must wait five weeks, not two. Many doctors miss this.
- Sertraline and escitalopram are the most commonly prescribed. They’re effective and generally safer, but they’re not risk-free.
Who’s Most at Risk?
It’s not just people on multiple antidepressants. The biggest danger zone is older adults.- 21.5% of Americans over 60 take an SSRI.
- 18.3% take an opioid for chronic pain.
- 22% of people over 65 take five or more medications daily.
What Should You Do?
If you’re on an SSRI, here’s what you need to know:- Never start a new medication, supplement, or herb without telling your doctor you’re on an SSRI. This includes over-the-counter cough syrups. Many contain dextromethorphan.
- Know the 5 S’s: Shivering, Sweating, Stiffness, Seizures (rare), Sudden confusion. If you notice any of these after starting a new drug, go to the ER.
- Don’t stop your SSRI suddenly. Withdrawal can mimic serotonin syndrome symptoms and cause severe anxiety, dizziness, and brain zaps. Always taper under medical supervision.
- Ask your pharmacist to review all your meds. They’re trained to spot dangerous combinations. Use their service-it’s free.
- Keep a written list of everything you take. Include doses and why you take them. Bring it to every appointment.
What’s Changing in 2025?
The system is finally catching up. In 2024, the FDA mandated that all electronic prescribing systems must include automatic alerts when a doctor tries to prescribe a high-risk combo-like an SSRI with tramadol or linezolid. Hospitals using Epic Systems saw a 32% drop in dangerous prescriptions after this update. The European Medicines Agency is also close to approving a blood test called SerotoninQuant, which could confirm serotonin syndrome within hours instead of relying on symptoms alone. That’s huge. But until then, the responsibility is still on you.Bottom Line
SSRI antidepressants save lives. But they’re not risk-free. The danger isn’t the drug itself-it’s what you mix it with. Thousands of people are hospitalized every year because someone didn’t know that a common painkiller could turn a safe medication into a life-threatening one. If you’re on an SSRI, treat every new medication like a potential trigger. Ask questions. Double-check. Don’t assume your doctor knows everything you’re taking. And if you feel something’s off-go to the hospital. Serotonin syndrome gets worse fast. Early treatment saves lives.Can you get serotonin syndrome from just one SSRI?
Rarely. Serotonin syndrome almost always happens when you combine SSRIs with another serotonergic drug-like an opioid, another antidepressant, or an herbal supplement. Taking a single SSRI at the right dose is very unlikely to cause it. The risk comes from drug interactions, not the medication alone.
How long should you wait after stopping an SSRI before starting an MAOI?
It depends on the SSRI. For most SSRIs, you need a 2-week washout period. But if you’re taking fluoxetine (Prozac), you must wait at least 5 weeks because it stays in your body so long. Skipping this step can be deadly. Always follow your doctor’s exact instructions.
Is tramadol safe if I’m on an SSRI?
No. Tramadol is one of the highest-risk combinations with SSRIs. It increases serotonin syndrome risk by nearly five times. Even if you’ve taken it before without issues, the risk builds over time. The CDC and FDA both recommend avoiding tramadol entirely if you’re on an SSRI. Use morphine, oxycodone, or acetaminophen instead for pain.
Can St. John’s wort cause serotonin syndrome with SSRIs?
Yes. St. John’s wort is a powerful serotonin booster and can trigger serotonin syndrome when taken with SSRIs. Many people think herbal supplements are safe because they’re "natural," but that’s false. The FDA has issued warnings about this combo for years. Stop using it immediately if you’re on an SSRI.
What should you do if you suspect serotonin syndrome?
Go to the emergency room immediately. Don’t wait. Symptoms like high fever, muscle rigidity, rapid heartbeat, or confusion can worsen within hours. Stop taking all serotonergic drugs right away. Treatment includes stopping the offending drugs, cooling the body, giving benzodiazepines for agitation, and sometimes serotonin blockers like cyproheptadine. Time is critical.
Are there any safe painkillers to take with SSRIs?
Yes. Morphine, oxycodone, codeine, and buprenorphine are considered low-risk when used with SSRIs. Acetaminophen (Tylenol) and NSAIDs like ibuprofen are also safe options for mild to moderate pain. Avoid tramadol, dextromethorphan, and meperidine entirely. Always check with your pharmacist before taking any new pain medication.
Can serotonin syndrome be fatal?
Yes. While many cases are mild and resolve quickly with treatment, severe cases can lead to organ failure, seizures, and death. The mortality rate for untreated or delayed-treated serotonin syndrome is high. When MAOIs are combined with SSRIs, the death rate can be 30-50%. Even with treatment, serious cases require ICU care. Never ignore the symptoms.




Donna Peplinskie
January 2, 2026 AT 05:51Just wanted to say thank you for writing this. I’m on sertraline, and my mom started taking St. John’s wort last year after reading a blog post that called it ‘nature’s Prozac.’ She didn’t tell her doctor. I found out when she called me at 2 a.m. shaking and sweating, convinced she was having a stroke. We rushed her to the ER. They said it was serotonin syndrome. She’s fine now, but I’ve been emailing every relative I know about this post. Please, if you’re on an SSRI-don’t trust ‘natural’ labels. Nothing in your body cares if it’s from a plant or a lab.
Also, pharmacists are heroes. My local one caught a tramadol interaction I didn’t even know was a thing. She printed me a list. I carry it in my wallet now.
Olukayode Oguntulu
January 3, 2026 AT 08:38Ah, the pharmacological hegemony rears its serotonin-laden head. You speak of risk as if it were a quantifiable variable, when in truth, the entire pharmacological paradigm is a construct of corporate interests masquerading as medical science. The FDA’s ‘warnings’? A regulatory theater designed to maintain the illusion of control. The real danger isn’t tramadol-it’s the epistemological arrogance of believing we can map the neurochemical sublime with algorithmic alerts and black-boxed pharmacokinetics.
Perhaps the answer isn’t more warnings, but less reliance on the pharmacopoeia altogether. The body is not a machine. It is a flux. To treat it as such is to invite collapse.
jaspreet sandhu
January 3, 2026 AT 15:09This is why people in America die from simple things. Everyone takes too many pills. In India, we don’t need all this science. If you feel bad, you eat turmeric, drink warm water, and sleep. No one mixes drugs. No one even knows what serotonin is. But we live longer than you. Why? Because we don’t trust pills. You have 276 million prescriptions and still you are sick. I am not surprised. You think a computer can tell you what your body needs? No. Your body knows. You just don’t listen. Stop taking so many things. One pill. That’s all. Not five. Not ten. One.
Also, St. John’s wort is just a plant. You think your body can’t handle a plant? You are weak.
Alex Warden
January 4, 2026 AT 21:11Let me guess-you’re one of those people who thinks the government has your best interests at heart. You believe these FDA alerts are there to protect you? Please. They’re there to protect the drug companies from lawsuits. The real reason tramadol got flagged is because generic opioids are cheaper and the pharma giants don’t want you switching. They want you on their branded SSRIs and their branded painkillers. The whole thing’s a racket.
And don’t even get me started on ‘pharmacist reviews.’ That’s just a front for insurance companies to push their preferred meds. Your ‘free’ pharmacist review? They’re paid to steer you toward the drugs that earn the most kickbacks. Wake up. This isn’t medicine. It’s capitalism with a stethoscope.
LIZETH DE PACHECO
January 6, 2026 AT 19:10This is exactly the kind of info I wish I’d had when I started my SSRI. I was 24, scared, and took everything at face value. I didn’t even know to ask about supplements. I took melatonin with my escitalopram for months-no one told me it could be risky. I’m so glad you laid this out so clearly. I’m sharing this with my book club. And yes, I now have a printed med list in my purse. No shame in being prepared.
Also, if you’re reading this and you’re on an SSRI-please, just talk to your pharmacist. They’re not there to judge. They’re there to help. I used to be embarrassed to ask. Now I bring them cookies. Seriously. They remember me. It matters.
Lee M
January 8, 2026 AT 02:56Stop being so dramatic. Serotonin syndrome is rare. You’re scaring people for clicks. I’ve been on fluoxetine for 12 years. Took tramadol for a back injury. No issues. My cousin took Prozac and St. John’s wort for six months. Fine. You’re turning a statistical outlier into a panic. People need pain relief. You can’t just say ‘avoid tramadol’ and call it a day. That’s not medicine. That’s fearmongering.
And why are you blaming the patient? The system’s broken. Doctors don’t have time. But you’re not offering solutions-you’re just adding to the noise.
Kristen Russell
January 8, 2026 AT 21:36One sentence: If you’re on an SSRI and start feeling weird after a new med-go to the ER. Don’t wait. Don’t Google. Go.
And yes, your pharmacist is your friend. Say hi. Bring them a coffee. They know more than your doctor sometimes.
Bryan Anderson
January 10, 2026 AT 09:54Thank you for the comprehensive overview. I work in primary care and see this every week-patients on multiple medications, often prescribed by different providers, with no centralized review. The 47% reduction in serotonin syndrome events with pharmacist-led reviews is a compelling statistic, and it underscores a critical gap in our current model of care.
It’s worth noting that many elderly patients are unaware that over-the-counter cough syrups contain dextromethorphan. We’ve started including a simple checklist in our intake forms: ‘Are you taking any supplements, OTC meds, or herbal remedies?’ It’s small, but it catches things. I’ve personally seen three cases of potential interactions avoided this way in the last six months.
Also, the half-life differences between SSRIs are under-taught in med school. Fluoxetine’s 15-day metabolite is a silent trap. I now make a point to write it down for patients switching meds. It’s not just a footnote-it’s a safety net.
Matthew Hekmatniaz
January 12, 2026 AT 02:52I’m from Iran, and we’ve been using St. John’s wort for depression for centuries-long before it was trendy in the West. But here’s the thing: we never mixed it with other antidepressants. We used it alone, or we used nothing at all. The cultural context matters.
What I find interesting is how Western medicine treats every interaction as a binary risk-safe or dangerous-when in reality, it’s a spectrum. Dose, timing, metabolism, age, liver function-all these things matter. A 70-year-old on multiple meds? Different story than a 25-year-old healthy person.
I’m not saying ignore the warnings. I’m saying: understand them. Don’t just memorize lists. Ask: ‘Why is this risky?’ Then you can make a real decision-not just a rule-following one.
Liam George
January 13, 2026 AT 01:33They’re lying to you. All of it. The FDA? Controlled by Big Pharma. The pharmacists? They’re paid by the same corporations that make the SSRIs. That ‘SerotoninQuant’ blood test? It doesn’t exist. It’s a psyop to make you think science is on your side. The real danger isn’t tramadol-it’s the neural surveillance they’re building. They want you dependent on pills so they can track your brain chemistry through your prescriptions.
And why is fluoxetine’s half-life so long? Because they engineered it that way. To keep you hooked. The ‘five-week washout’? A trap. You think that’s for your safety? It’s to ensure you never stop. They want you on it forever.
Don’t take anything. Don’t trust anyone. Your body can heal itself. They just don’t want you to know that.
Donna Peplinskie
January 14, 2026 AT 12:20Hey, I just read your comment about the blood test being fake. I actually work in a lab that’s helping pilot SerotoninQuant. It’s real. We’re validating it with 12 hospitals right now. I know it sounds crazy, but it’s happening. I’ve seen the data.
And no, they didn’t engineer fluoxetine to keep you hooked. That’s not how drug development works. It’s just how the molecule behaves. I wish it were simpler. But it’s not a conspiracy. It’s chemistry.
Thanks for caring enough to worry. Just… maybe check your sources before assuming the worst. We’re all trying to stay safe here.