Generic Medication Excipient Checker
Check if your sensitivities could affect generic medications
This tool helps you understand if your known allergies or sensitivities might cause side effects when switching to generic medications.
Your Results
Recommended Actions
- Check the package insert for complete ingredient list
- Ask your pharmacist about specific excipients
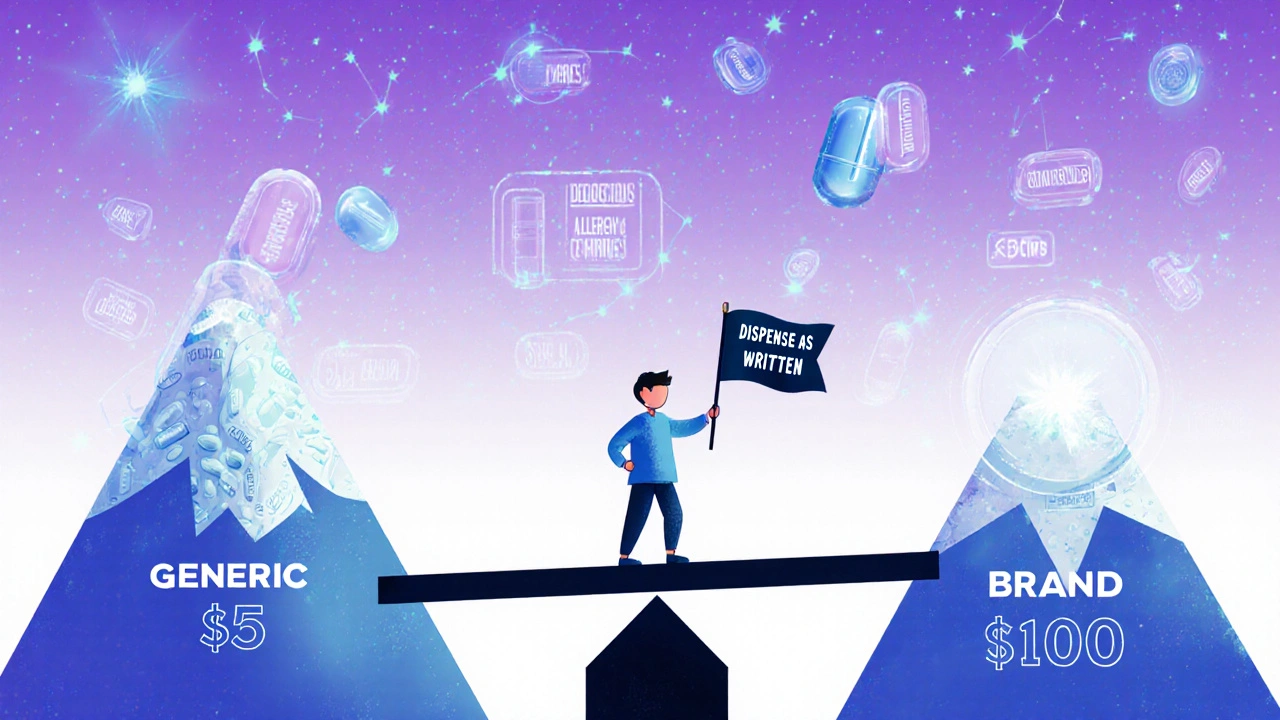
- Consider requesting "Dispense as Written" on prescription
- Track your reactions in a medication log
When you pick up a prescription, you might not notice the difference between a brand-name pill and its generic version. They look similar, cost far less, and your doctor says they’re the same. But for some people, that small difference in excipients-the inactive ingredients-can mean the difference between feeling fine and feeling awful.
What Exactly Are Excipients?
Excipients aren’t the part of the medicine that treats your condition. They’re the fillers, binders, dyes, and preservatives that help the drug hold its shape, dissolve properly, or taste better. Think of them like the packaging and delivery system for the active ingredient. A tablet might contain lactose as a filler, croscarmellose sodium to help it break apart, or FD&C Red No. 40 for color. These ingredients are safe for most people. But for someone with a sensitivity, even a tiny amount can cause problems.The FDA requires generic drugs to have the same active ingredient, strength, and dosage form as the brand-name version. That part is non-negotiable. But when it comes to excipients? Manufacturers have freedom. One company might use corn starch. Another might use potato starch. One might add lactose. Another might skip it entirely. And that’s where things get tricky.
Why Do Some People React to Generic Medications?
Most people switch from brand to generic without a hitch. In fact, 78% of users report no difference at all. But for the 12% who do notice something off, the culprit is often excipients-not the active drug.Take lactose intolerance. A generic version of a heart medication might contain lactose as a filler. If you’re lactose intolerant, that small amount can trigger bloating, cramps, or diarrhea. Those symptoms aren’t from the drug itself-they’re from the filler. And because they show up after a switch, patients often think the medication isn’t working, not that their body is reacting to something new.
Another example: croscarmellose sodium, a common disintegrant in tablets. One patient with a rare allergy to this ingredient had a severe reaction after switching from branded furosemide to a generic version. The active ingredient was identical. The problem? The generic used a different excipient blend. The reaction stopped only after switching back.
For people with autoimmune conditions, food allergies, or sensitivities to dyes and preservatives, these hidden ingredients matter. The American Autoimmune Related Diseases Association has documented cases where patients with celiac disease reacted to gluten traces in fillers, or those with histamine intolerance had flare-ups from certain preservatives in generic thyroid meds.
Narrow Therapeutic Index Drugs: When Small Changes Matter
Not all medications are created equal when it comes to switching. Some drugs have what’s called a narrow therapeutic index-meaning the difference between a dose that works and one that’s toxic is very small.Examples include:
- Warfarin (blood thinner)
- Levothyroxine (thyroid hormone)
- Phenytoin and carbamazepine (anti-seizure drugs)
- Cyclosporine and tacrolimus (immunosuppressants)
For these, even a 5% change in how quickly the drug enters your bloodstream can lead to treatment failure or dangerous side effects. While generics must meet strict bioequivalence standards (90-110% for NTI drugs, not the usual 80-125%), excipients can still affect how fast the pill dissolves in your gut. A slower-dissolving tablet might delay absorption, causing your drug levels to dip below the effective range. A faster-dissolving one might spike levels, increasing side effects.
Parkinson’s patients have reported this firsthand. On the Michael J. Fox Foundation’s patient platform, 18% of 5,247 respondents said their symptoms worsened after switching from branded levodopa to a generic. One Reddit user wrote: “I went from having 3 good hours after my dose to 45 minutes. Switched back to Sinemet-back to normal.” The issue wasn’t the levodopa. It was the binder and coating used in the generic version, which changed how quickly it dissolved.
What Does the Science Say?
A 2022 study in JAMA Internal Medicine looked at 47 drug classes and found that 92% of generics performed just as well as brand-name drugs. That’s reassuring. But the remaining 8% showed measurable differences in outcomes-mostly in those narrow therapeutic index categories.Research from the Journal of Clinical Pharmacy and Therapeutics (March 2024) found that 68% of adverse events linked to generic switches could have been predicted if patients had been screened for excipient intolerances beforehand. That’s a huge red flag. If we knew who was sensitive to lactose, dyes, or certain fillers, we could avoid these problems before they happen.
The FDA itself acknowledges this. In a 2023 report, they admitted that while generic drugs are safe and effective for the vast majority, “rarely, differences in inactive ingredients can cause issues for specific patients.”
How to Protect Yourself
If you’ve had a bad reaction after switching medications, you’re not imagining it. Here’s what you can do:- Track your reactions. Keep a simple log: date, medication name, dose, and any new symptoms. Note if they started after a switch.
- Ask your pharmacist. Pharmacists have access to the full ingredient list. Ask: “Does this generic contain lactose, FD&C dyes, or gluten?”
- Check the package insert. The small booklet inside your pill bottle lists all ingredients-active and inactive. Don’t skip it.
- Ask your doctor to write “Dispense as Written” or “Do Not Substitute.” This legally prevents the pharmacy from swapping your brand for a generic.
- Stick with the same generic manufacturer. If you find a generic that works, try to refill with the same brand of generic. Manufacturers change formulations without warning.
Many people don’t realize they can request the brand-name version. Insurance may charge more, but if your health depends on it, it’s worth pushing back. Medicare Part D plans often cover generics at $1-$5 co-pays, while brand-name versions can cost $40-$100. But for some, that extra cost is the price of stability.
The Bigger Picture
Generic drugs save the U.S. healthcare system about $373 billion a year. That’s huge. But the system was built on the assumption that all patients are the same. They’re not.The FDA is starting to take excipient differences more seriously. In 2024, they launched a plan to create a public database listing all excipients in brand and generic drugs. Generic manufacturers are also beginning to standardize ingredients in high-risk drugs-like levodopa and warfarin-to reduce switching problems.
By 2030, “clean excipient profiles” may become a selling point for generic makers, just like “gluten-free” or “non-GMO” on food labels. For patients with sensitivities, this could be a game-changer.
Right now, the burden falls on you. If you’ve had a bad reaction, speak up. Talk to your pharmacist. Ask your doctor to document your intolerance. Your experience isn’t rare-it’s a signal that the system needs to adapt.
What’s Next?
If you’re on a medication with a narrow therapeutic index-or you have known allergies to dyes, lactose, or gluten-don’t assume generics are always safe. Keep a record. Know your ingredients. And don’t be afraid to ask for what works for your body.The goal isn’t to stop generics. It’s to make them safer for everyone-including the 15 to 20 million Americans who have significant excipient intolerances. You deserve a medication that doesn’t just treat your condition, but also respects your body’s limits.
Can generic medications cause side effects that the brand-name version doesn’t?
Yes, but not because of the active ingredient. Side effects from generics are usually caused by differences in inactive ingredients, or excipients, like lactose, dyes, or preservatives. A patient who is lactose intolerant might experience bloating or diarrhea after switching to a generic version that contains lactose as a filler, even though the drug itself is unchanged.
Are all generic drugs the same?
No. While all generics must contain the same active ingredient at the same strength, different manufacturers use different excipients, coatings, and manufacturing processes. Two generic versions of the same drug can have different fillers or dissolution rates, which can affect how quickly the drug is absorbed-especially important for narrow therapeutic index medications.
Which medications are most likely to cause problems when switched to generic?
Medications with a narrow therapeutic index are most sensitive to changes. These include levothyroxine (for thyroid), warfarin (blood thinner), phenytoin and carbamazepine (anti-seizure), cyclosporine (immunosuppressant), and levodopa (for Parkinson’s). Small changes in absorption can lead to treatment failure or dangerous side effects.
How can I find out what’s in my generic medication?
Check the package insert that comes with your prescription-it lists all active and inactive ingredients. You can also ask your pharmacist for the full ingredient list. Online databases like the FDA’s upcoming excipient database will eventually make this easier, but for now, direct communication with your pharmacist is your best tool.
Can I request the brand-name drug instead of a generic?
Yes. Your doctor can write “Dispense as Written” or “Do Not Substitute” on your prescription. This legally prevents the pharmacy from substituting a generic. Insurance may require you to pay more, but if you’ve had a bad reaction to a generic, your health comes first.
Why don’t pharmacies tell me what excipients are in my medication?
Pharmacies aren’t required to list excipients on the label, and most don’t have the time to explain them. The information is in the package insert, but many patients don’t read it. Pharmacists can provide the details if you ask-so always ask. Your awareness can prevent a bad reaction.
Is it safe to switch back and forth between brand and generic?
For most people, yes. But if you’re on a narrow therapeutic index drug or have known excipient sensitivities, frequent switching can cause instability in your condition. Stick with one version-brand or generic-and avoid unnecessary switches. Consistency matters more than cost in these cases.





Dion Hetemi
November 19, 2025 AT 14:41Man, I switched to a generic warfarin last year and ended up in the ER because my INR spiked. Turned out the generic used a different filler that made it absorb too fast. My pharmacist didn’t even blink when I asked. Had to go back to brand-name and pay $90 a month. Worth it. Don’t let them bullsh*t you into thinking it’s all the same.
Kara Binning
November 20, 2025 AT 02:54Oh please. This is just another ‘I’m special’ cry for attention. The FDA approves these drugs. If you can’t handle a little lactose or dye, maybe you’re the problem, not the system. Stop being a liability to healthcare cost savings.
Michael Petesch
November 20, 2025 AT 13:48While the anecdotal evidence presented is compelling, it’s critical to contextualize it within the broader pharmacoeconomic landscape. The 8% of cases showing measurable differences in outcomes predominantly involve narrow therapeutic index drugs, where bioequivalence thresholds are already more stringent. The real issue lies in the absence of standardized excipient disclosure across manufacturers - a regulatory gap, not a failure of generic science.
Andrew Montandon
November 21, 2025 AT 00:04Hey everyone - I’ve been a pharmacist for 18 years, and I’ve seen this exact thing happen over and over. A patient comes in screaming their thyroid meds ‘stopped working’ - turns out the new generic had dyes they’re allergic to. We check the insert, swap back, and boom - they’re fine. Please, please, please ask your pharmacist for the full ingredient list. It’s right there in the package insert - no magic, just legwork. And if you’re on levothyroxine or warfarin? Stick with the same brand of generic. Don’t let the pharmacy switch it randomly. You’re not being difficult - you’re being smart.
Sam Reicks
November 21, 2025 AT 18:57the fda is lying to you. theyre in bed with big pharma. generics are just placebos with the same active ingredient. theyre slowly replacing everything with corn syrup and microplastics. you think your heart med is safe? think again. theyre testing on you. and the labels? totally fake. dont trust any pill you didnt make yourself
Chuck Coffer
November 23, 2025 AT 17:42So let me get this straight. You’re telling me that after 50 years of generic drugs being used by millions, suddenly a handful of people are having ‘issues’ because they didn’t read the tiny print? Maybe the problem isn’t the pill - it’s the expectation that someone else should do your homework.
Paige Lund
November 25, 2025 AT 09:01Wow. So much text. So little actual impact. I switched generics last week. Still alive. Still taking pills. Still not crying about it.
Reema Al-Zaheri
November 27, 2025 AT 03:35The scientific literature is unequivocal: bioequivalence standards for narrow therapeutic index drugs are rigorously enforced. However, the absence of mandatory excipient labeling remains a critical oversight. The proposed FDA database is a necessary step, but it must be publicly accessible, machine-readable, and updated in real time. Without transparency, patient autonomy is compromised.
Michael Salmon
November 29, 2025 AT 02:09Everyone’s acting like this is some new revelation. It’s not. I’ve been warning people for years - generics are a gamble. The only reason they’re allowed to change fillers is because no one checks. The FDA doesn’t care. Your doctor doesn’t care. Your pharmacist? They’re too busy ringing up your $5 co-pay. You think you’re saving money? You’re just trading stability for a discount.
Joe Durham
November 29, 2025 AT 22:25I get it - this stuff matters. I have a friend with celiac who had a flare-up after switching to a generic version of her seizure med. Turns out, the filler had trace gluten. She didn’t know until she pulled the insert. We all assumed it was ‘just inactive.’ But for her, it was life-changing. Maybe the real issue isn’t generics - it’s that we don’t treat patients like individuals. We treat them like data points.
Derron Vanderpoel
December 1, 2025 AT 16:50I switched my Parkinson's med to generic and my hands started shaking like I was holding a cup of coffee after three espressos. I thought I was dying. I went back to Sinemet and - poof - calm again. I cried. Not because I’m weak - because I felt like nobody listened. This isn’t just about pills. It’s about being heard.
Timothy Reed
December 3, 2025 AT 08:23This is an excellent and necessary discussion. The healthcare system prioritizes cost-efficiency over individualized care - and that’s a structural flaw. The solution isn’t to eliminate generics, but to mandate excipient transparency and allow patients to opt out of substitutions based on documented sensitivities. Pharmacists should be empowered to flag high-risk switches. We can save money and still respect patient safety - it just requires policy updates.
Christopher K
December 4, 2025 AT 17:38USA: 373 billion saved on generics. Europe: 400 billion. China: 200 billion. And yet, somehow, only Americans are having ‘excipient trauma.’ Coincidence? Or is it just that we’re too soft to handle a little lactose? Maybe we need less medicine and more grit.
Angela Gutschwager
December 6, 2025 AT 13:20My mom had a reaction to a generic thyroid med. Turns out it had FD&C Yellow No. 5. She’s allergic. We switched back. Cost: $80 more/month. Worth it. 🙃