For years, if you had back pain, a doctor or physiotherapist would show you an X-ray or MRI and say, "Your disc is bulging. That’s what’s hurting you." You were told to avoid movement, rest, and maybe take pills. But what if that explanation was wrong? What if the pain wasn’t coming from damaged tissue at all - but from your brain misreading signals? This isn’t science fiction. It’s pain neuroscience education - and it’s changing how thousands of people live with long-term pain.
Why Your Pain Isn’t Always a Signal of Damage
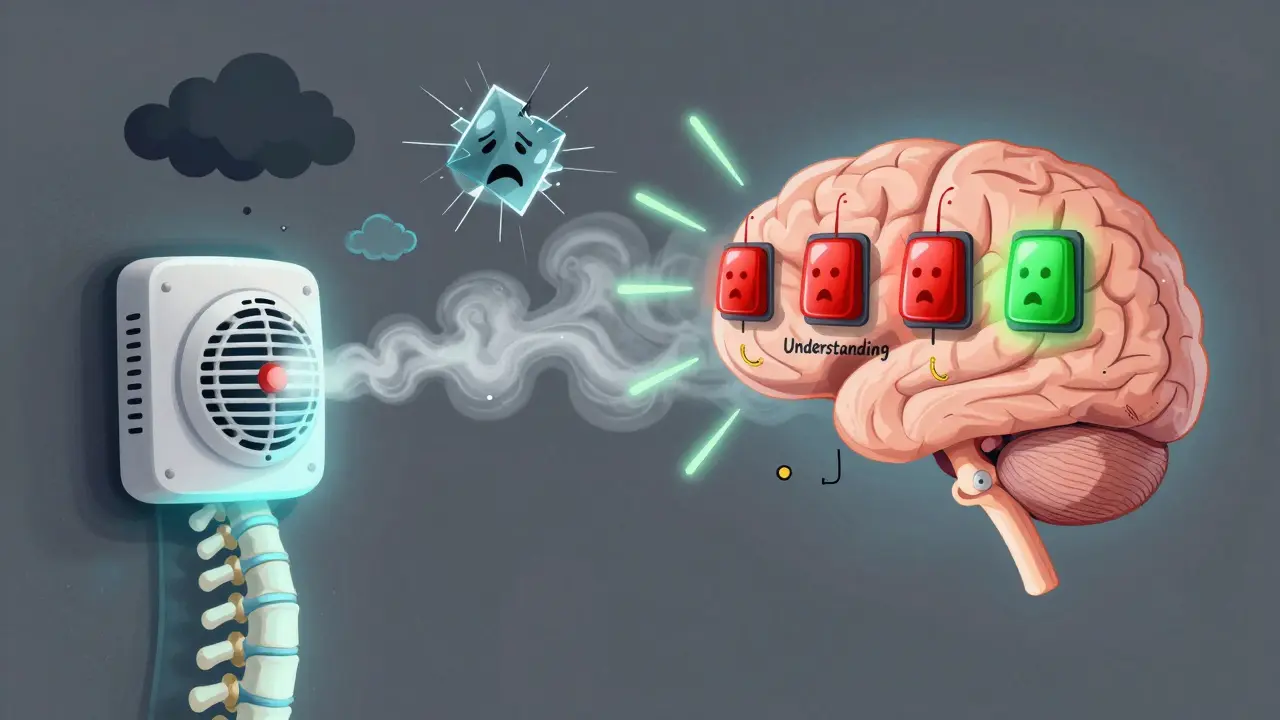
Most people think pain works like a simple alarm. If you hurt your knee, the injury sends a signal to your brain, and your brain says, "Ouch!" That makes sense. But when pain sticks around for months or years - even after tissues have healed - that model falls apart. That’s where pain neuroscience education comes in. Pain isn’t a direct measurement of tissue damage. It’s a protective output from your brain. Think of it like a smoke alarm. If the alarm goes off because you burned toast, that’s useful. But if it goes off every time the humidity rises, even when there’s no fire - that’s a problem. Your nervous system can become overly sensitive. This is called central sensitization. Your brain starts interpreting normal sensations - like walking, bending, or even a light touch - as dangerous. That’s not because your body is broken. It’s because your brain has learned to be too cautious. This shift in thinking isn’t just theory. A 2023 review of 23 clinical trials found that people who received pain neuroscience education saw an average drop of 1.8 points on a 10-point pain scale. That’s not just statistically significant - it’s life-changing. For someone who’s been in pain for years, going from an 8 to a 6 isn’t a small win. It’s the difference between staying in bed and playing with your grandkids.How Pain Neuroscience Education Works
Pain neuroscience education, or PNE, isn’t a treatment like a massage or a stretch. It’s a conversation - a way of helping your brain understand that it’s overreacting. A typical session lasts 30 to 45 minutes. It’s usually done one-on-one by a physical therapist, but sometimes in small groups. The goal? To replace fear with understanding. Practitioners use simple metaphors. One of the most common is the "sensitive smoke alarm." Another is comparing pain to a "stuck thermostat." Your brain used to be perfectly calibrated. But after injury, stress, or long-term inactivity, it got turned up too high. The education helps you see that your pain isn’t a sign of damage - it’s a sign of your nervous system being on high alert. The science behind this is solid. fMRI studies show that after PNE, activity drops in brain areas linked to threat detection - like the insula and amygdala. At the same time, areas responsible for reasoning and control - like the prefrontal cortex - become more active. In short: your brain starts to trust your body again. This isn’t just about feeling less pain. It’s about feeling more capable. The same 2023 review showed a 12.3% reduction in disability scores. People reported being able to walk further, sleep better, and return to hobbies they’d given up. One patient, a 42-year-old nurse with fibromyalgia, cut her daily pain medication from six pills to just one every three days after six sessions of PNE combined with graded movement. That’s not magic. That’s neuroscience.What PNE Is Not
It’s important to know what PNE doesn’t do. It won’t erase pain overnight. It won’t fix structural issues like arthritis or disc degeneration. And it’s not a replacement for movement, exercise, or manual therapy - it’s a powerful partner to them. Studies show PNE alone improves pain and function. But when combined with exercise or hands-on therapy, results jump by 30-40%. That’s because PNE removes the fear that stops people from moving. Once fear drops, movement becomes safe again. And movement is what actually rebuilds strength, reduces sensitivity, and reprograms the nervous system. PNE also doesn’t work for everyone. It’s less effective for acute pain - like after surgery or a recent injury - where tissue damage really is the main problem. It’s also harder for people with low health literacy or cognitive impairment. If someone can’t grasp the idea that pain isn’t always danger, the education won’t stick. That’s why good practitioners tailor their language. Instead of saying "neuroplasticity," they say "your brain can learn new patterns." Instead of "peripheral sensitization," they say "your nerves are on edge."
Why Traditional Pain Education Falls Short
Traditional pain advice often says things like: "Don’t lift that. It’ll make your back worse." Or: "Your spine is worn out. You’ll always have pain." These messages reinforce fear. They tell your brain that your body is fragile. That’s the opposite of what you need. One 2022 review compared PNE to traditional biomedical education in people with chronic low back pain. The PNE group improved by 4.7 points on a disability scale. The traditional group? Just 1.2 points. That’s a four-point gap - and it’s not because one group worked harder. It’s because one group was told their body was broken, and the other was told their brain was being too cautious. Even more telling: when PNE was added to standard physiotherapy, pain scores dropped by 10.8 points on a 100-point scale. Without PNE, the drop was only 5.3. That’s more than double the benefit. And when compared to placebo education - where patients got generic advice like "stay active," without any science - PNE reduced pain catastrophizing by 35%. Catastrophizing means thinking the worst: "This will never get better," "I’m ruined," "I’ll be in pain forever." PNE breaks that cycle.Who Delivers PNE and How to Get Started
You won’t find PNE in every clinic - yet. But it’s growing fast. In the U.S., 68% of physical therapy clinics that specialize in pain now use it. In the UK, it’s less common, but gaining ground. The best practitioners are physical therapists, occupational therapists, or pain psychologists who’ve taken specialized training. There’s no official certification, but the International Spine and Pain Institute offers a 24-hour course that’s widely respected. Many clinicians spend 3 to 6 months learning how to explain these concepts clearly. It’s not just about knowing the science - it’s about knowing how to talk about it without overwhelming people. If you’re interested, ask your therapist: "Do you use pain neuroscience education?" If they look confused, ask if they’ve read "The Explain Pain Handbook" by David Butler and Lorimer Moseley. If they haven’t heard of it, they may not be trained in it. You can also look for digital tools. The Pain Revolution app, used by over 186,000 people, walks users through PNE concepts with animations and stories. It’s not a replacement for a good therapist, but it’s a great supplement.
Real Stories, Real Change
On Reddit’s chronic pain community, one user named PainWarrior87 wrote: "After six months of fearing movement would damage my back, the metaphor of a sensitive smoke alarm helped me understand my pain wasn’t signaling danger. I’ve since returned to hiking and reduced opioid use by 75%." That’s the power of understanding. Another case: a 58-year-old teacher with chronic neck pain had been told she had "severe degeneration" on her MRI. She avoided turning her head, feared car rides, and stopped gardening. After four sessions of PNE, she learned her spine wasn’t crumbling - it was just hypersensitive. She started gentle neck movements. Within three months, she was back in her garden. Her pain didn’t vanish. But it stopped controlling her. Not everyone has a success story. About 17% of patients in online reviews say PNE didn’t help. The most common complaints? "Too much science," and "I expected the pain to disappear." That’s the biggest hurdle. PNE isn’t a quick fix. It’s a rewiring. And rewiring takes time, patience, and trust.What’s Next for Pain Neuroscience Education
PNE is expanding beyond chronic pain. Researchers are now testing it for post-surgical recovery, acute injuries, and even in hospitals to reduce opioid use after operations. A major NIH-funded trial is underway to see if PNE can help people recover faster after spine surgery. New tools are coming too. Virtual reality programs are being tested to teach PNE in immersive, engaging ways. Early results show 30% better knowledge retention than traditional methods. And some clinics are starting to use wearable sensors to show patients how their nervous system responds to movement - turning abstract science into real-time feedback. The biggest challenge? Training enough clinicians. Only 28% of physical therapists in the U.S. feel confident delivering PNE. That’s why more universities are adding it to their curricula. In 2010, only 12% of U.S. programs taught it. By 2023, that number jumped to 72%. And insurance is catching up. Since 2021, Medicare in the U.S. has started reimbursing PNE as part of physical therapy visits. That means more people can access it without paying out of pocket.What You Can Do Today
If you’ve been living with long-term pain and feel stuck, here’s what to try:- Ask your therapist if they use pain neuroscience education. If not, ask if they’re open to learning it.
- Read "The Explain Pain Handbook" - even just the first chapter. It’s written for patients, not doctors.
- Download the Pain Revolution app. It’s free to try, and it breaks down complex ideas into simple stories.
- Stop avoiding movement because you’re afraid it’ll hurt. Pain doesn’t always mean damage. Try gentle movement - even if it aches a little. That’s how your brain learns it’s safe.
- Write down your pain beliefs. Do you think your spine is broken? Your nerves are frayed? Your body is failing? Challenge them with what you learn.




Philip House
January 21, 2026 AT 12:31Look, I get it - your brain’s a ‘smoke alarm’ now? Cool story. But let’s be real: if your spine’s degenerated from 40 years of lifting boxes and sitting on your ass, no amount of ‘neuroscience’ is gonna make that MRI look clean. You’re not ‘overreacting’ - your body’s just old. Stop trying to psych yourself out and just accept that some damage is permanent. Pain ain’t a bug, it’s a feature of being human.
Akriti Jain
January 23, 2026 AT 04:16OMG this is SOOOO 2023 😭✨ the elite are using PNE to make us think pain is ‘all in our heads’ so we don’t sue Big Pharma 🤫🧠 #MindControl #PainIsACon #TheyDontWantYouHealed
Mike P
January 23, 2026 AT 16:29Bro, this is why America’s healthcare system is winning. You don’t need some foreign therapist with a clipboard telling you your spine’s ‘fine’ - you need facts. And the facts? Your body’s a machine. If it’s broken, fix it. If it’s not, stop coddling yourself. PNE is just therapy for people who think crying into a yoga mat counts as exercise. I’ve been lifting since I was 14. My back’s seen worse than your ‘sensitive smoke alarm.’ Move. Lift. Don’t overthink it.
shivani acharya
January 25, 2026 AT 14:36Okay but let’s be honest - this whole PNE thing is just a fancy way to gaslight people who are in real pain. I’ve had fibro for 12 years. I’ve been told my pain is ‘just stress’ by doctors who’ve never touched a patient’s spine. Now they’re calling it ‘central sensitization’? That’s just a new word for ‘we don’t know what’s wrong so we’ll blame your brain.’ And don’t get me started on the app. ‘Pain Revolution’? More like ‘Pain Exploitation.’ They’re selling hope like it’s a subscription box. Meanwhile, my meds are still the only thing that lets me sleep. You can’t ‘retrain’ your brain when your nerves are screaming. And no, I don’t want to ‘try gentle movement.’ I want someone to fix me - not reprogram me.
Sarvesh CK
January 25, 2026 AT 22:19It is indeed a profoundly significant paradigm shift, one that aligns with the growing body of evidence in neurophenomenology and embodied cognition. The reduction in catastrophizing and the increased prefrontal engagement observed in fMRI studies suggest not merely a cognitive reframing, but a genuine neuroplastic reorganization. This is not a dismissal of somatic reality, but rather an expansion of it - recognizing that the nervous system, as a dynamic, context-sensitive organ, does not merely transmit signals but constructs experience. The metaphors employed - smoke alarm, thermostat - are not reductive; they are pedagogical bridges. Yet, one must remain cautious not to conflate explanatory efficacy with therapeutic omnipotence. The integration of PNE with graded motor imagery and somatosensory retraining remains the most empirically robust pathway forward. One must also acknowledge the cultural and linguistic barriers to its dissemination, particularly in contexts where biomedical reductionism remains culturally hegemonic.
Hilary Miller
January 26, 2026 AT 02:59My mom tried this after her hip surgery and now she’s gardening again. No magic, just science. 🌿
Lauren Wall
January 27, 2026 AT 15:09So now we’re blaming the brain because doctors used to be dumb? Great. Next they’ll say cancer is ‘just your cells being too emotional.’
Kenji Gaerlan
January 28, 2026 AT 00:14idk man i think this is just a bunch of hippy nonsense. my back hurts because i sat wrong for 10 years. not because my brain’s ‘overreacting.’ also i think they’re just tryna sell apps and books. 🤷♂️
Oren Prettyman
January 28, 2026 AT 10:18It is incumbent upon the reader to recognize the implicit epistemological bias embedded within this exposition: namely, the conflation of phenomenological experience with neurophysiological causation. The invocation of fMRI data as evidentiary validation is, in fact, a fallacy of neuroreductionism - one that presumes neural activity patterns are synonymous with subjective states. Furthermore, the dismissal of structural pathology as irrelevant is not merely unscientific, but ethically dubious. To assert that disc degeneration is ‘not a problem’ while simultaneously recommending movement as curative is a form of therapeutic nihilism masked as enlightenment. The data cited - while statistically significant - lack clinical generalizability, particularly in populations with comorbid autoimmune or neurodegenerative conditions. One must not mistake the pedagogical utility of metaphor for ontological truth. Pain, at its core, remains a biological alarm - even if it is occasionally false. To deny the integrity of tissue damage is to deny the very foundation of medicine.