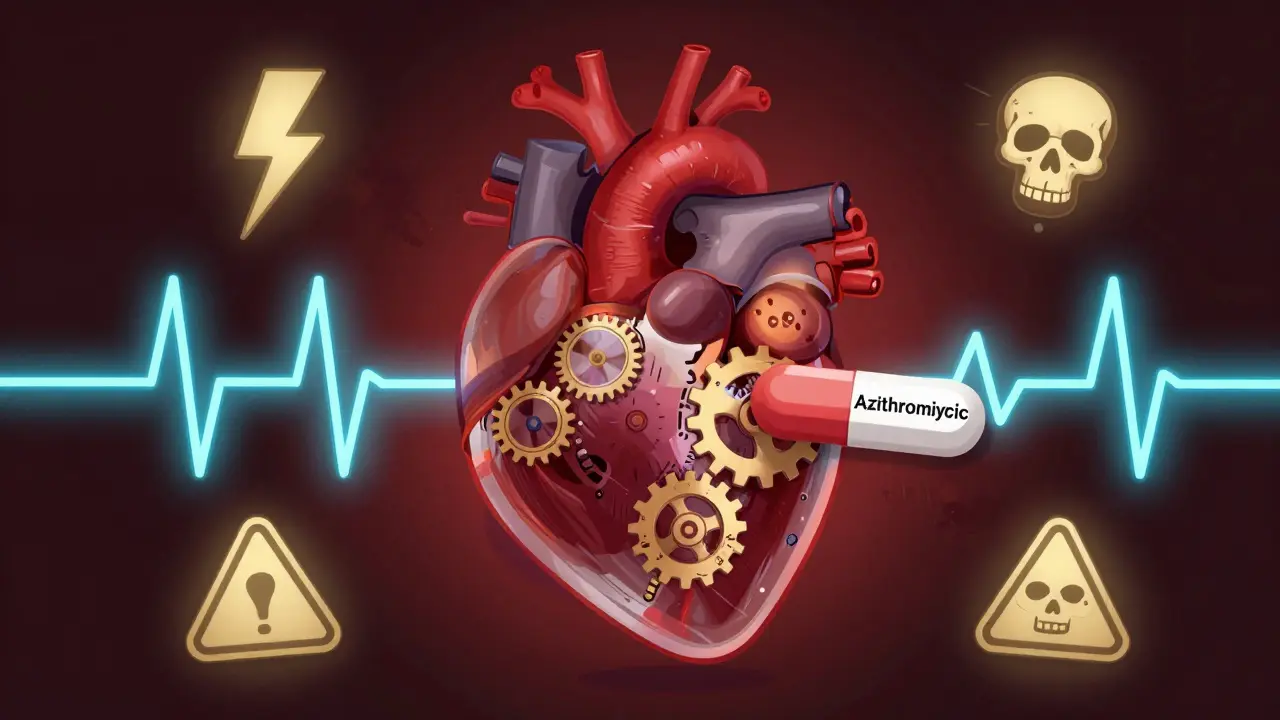
When you take an antibiotic for a stubborn sinus infection or bronchitis, you’re probably not thinking about your heart. But for some people, common antibiotics like azithromycin or clarithromycin can quietly disrupt the heart’s rhythm-sometimes with deadly results. This isn’t theoretical. It’s documented, studied, and tracked by the FDA, the American Heart Association, and hospitals across the U.S. and Europe. The issue? QT prolongation.
What Is QT Prolongation and Why Does It Matter?
Your heart beats because of electrical signals. These signals travel through heart muscle cells in a precise sequence: depolarization (the beat), then repolarization (the reset). The QT interval on an ECG measures how long this entire cycle takes. If it stretches too long-known as QT prolongation-the heart’s reset phase gets delayed. That creates a dangerous window where the heart can fire off random, chaotic signals. The result? A life-threatening arrhythmia called Torsades de pointes (TdP), which can spiral into sudden cardiac arrest. Macrolide antibiotics-like azithromycin, clarithromycin, and erythromycin-interfere with this reset. They block a specific potassium channel in heart cells called hERG (human ether-a-go-go-related gene). This channel normally helps the heart reset quickly after each beat. When it’s blocked, the electrical signal lingers. That’s QT prolongation. And it doesn’t take much: studies show that even a 60 ms increase from baseline can trigger TdP in vulnerable people.Not All Macrolides Are Created Equal
If you’ve been prescribed one of these antibiotics, you might be wondering: which one is safest? The answer isn’t simple, but the data is clear. Clarithromycin carries the highest risk. It doesn’t just block potassium channels-it also strongly inhibits CYP3A4, a liver enzyme that breaks down many drugs. That means it can cause other QT-prolonging medications (like certain antidepressants or antifungals) to build up in your system. The FDA requires a black box warning on clarithromycin labels for this reason. Erythromycin is less potent at blocking hERG, but it causes more stomach upset. Vomiting and diarrhea can lead to low potassium levels (hypokalemia), which independently increases arrhythmia risk. One study found hypokalemia triples the chance of TdP when combined with macrolides. Azithromycin was once considered the safest option. It barely affects CYP3A4 and has weaker hERG blockade. But that reputation shifted after a landmark 2012 study tracked 1.3 million prescriptions. Researchers found azithromycin was linked to a 2.85 excess death per 1,000 courses in the first five days compared to amoxicillin. The FDA added a warning, though not a black box. Real-world data shows it still causes TdP-especially when stacked with other QT-prolonging drugs like hydroxychloroquine during the pandemic.Who’s at Real Risk?
The good news? For most healthy adults, the risk is tiny. The bad news? It spikes dramatically in certain groups. Six major risk factors push someone into danger zone:- Female sex - 68% of TdP cases occur in women
- Age over 65 - 2.4 times higher risk
- Baseline QTc over 450 ms - 4.7 times higher risk
- Other QT-prolonging drugs - each additional drug increases risk by 1.8 times
- Low potassium or magnesium - hypokalemia triples the risk
- Heart failure or structural heart disease - 5.3 times higher risk

What Doctors Should Do (And What They Often Don’t)
Guidelines from the American College of Cardiology say: if you have two or more risk factors, get a baseline ECG before starting a macrolide. Repeat the ECG if the QTc goes above 470 ms in men or 480 ms in women-or if it increases by more than 60 ms from your baseline. But here’s the problem: most primary care doctors don’t do this. ECGs aren’t automatic. Risk assessments aren’t built into most prescription systems. A 2022 study found that fewer than 15% of Medicare patients with multiple risk factors received a pre-prescription ECG before being given clarithromycin. Even worse, some patients have what’s called “repolarization reserve” failure. Their QT interval looks normal, but they carry a hidden genetic mutation in their hERG channel. These people can have no family history of sudden death, no symptoms-until they take a macrolide. That’s why experts now recommend asking about unexplained fainting or sudden cardiac death in close relatives-even if the ECG looks fine.Alternatives and What to Ask Your Doctor
You don’t need a macrolide for most infections. For community-acquired pneumonia, doxycycline or amoxicillin-clavulanate are just as effective and carry no QT risk. For sinusitis, amoxicillin or cefdinir are first-line. For strep throat, penicillin or cephalexin are standard. If your doctor reaches for azithromycin or clarithromycin, ask:- “Is this the safest antibiotic for me, given my health history?”
- “Am I taking any other meds that could interact?”
- “Could I get an ECG before starting this?”
- “What are the signs of trouble? What should I do if I feel dizzy or my heart races?”
New Tools Are Helping-But They’re Not Everywhere
The field is catching up. In 2023, the FDA approved the CardioCare QT Monitor, a handheld ECG device that gives automated QTc readings with under 5 ms error. It’s used in some hospitals and urgent care centers-but not in most doctor’s offices. A bigger breakthrough? The Macrolide Arrhythmia Risk Calculator (MARC). Developed at Brigham and Women’s Hospital, it uses 12 variables-age, sex, meds, electrolytes, ECG, kidney function-to predict your personal TdP risk with 89% accuracy. It’s not in widespread use yet, but it’s changing how specialists approach prescribing. There’s also research into “cardiosafe” macrolides. Solithromycin showed 78% less hERG blockade than clarithromycin in trials-but was pulled due to liver toxicity. Scientists are now looking at genetic markers. Early data suggests 15% of people carry hERG variants that make them 4.2 times more sensitive to macrolide-induced QT prolongation. Future prescriptions might be personalized based on DNA.Bottom Line: Don’t Panic, But Don’t Ignore It
Macrolide antibiotics save lives. They’re cheap, effective, and widely used. But they’re not risk-free. The danger isn’t in the drug itself-it’s in the combination of the drug with your body’s unique vulnerabilities. If you’re young, healthy, and have no other meds, your risk is extremely low. But if you’re older, have heart issues, take other drugs, or have low potassium-this isn’t something to brush off. Ask questions. Get an ECG if recommended. Push back if your doctor dismisses your concerns. The goal isn’t to avoid antibiotics. It’s to use them wisely. Your heart is counting on it.Can azithromycin really cause a heart attack?
Azithromycin doesn’t directly cause heart attacks, but it can trigger Torsades de pointes, a dangerous arrhythmia that can lead to sudden cardiac arrest if not treated immediately. This is rare in healthy people but becomes much more likely in those with existing heart conditions, low potassium, or who are taking other QT-prolonging drugs. The 2012 JAMA study found a small but real increase in cardiovascular deaths within the first five days of azithromycin use compared to amoxicillin.
Is clarithromycin more dangerous than azithromycin?
Yes. Clarithromycin has stronger hERG channel blockade and inhibits the liver enzyme CYP3A4, which can raise levels of other heart-risky drugs in your system. It carries a black box warning from the FDA for QT prolongation and TdP. Azithromycin has a lower risk profile but still carries warnings, especially when combined with other medications or in high-risk patients.
Should I get an ECG before taking a macrolide antibiotic?
If you have two or more risk factors-like being over 65, female, on diuretics, having heart failure, or taking other QT-prolonging drugs-yes. Guidelines from the American College of Cardiology recommend a baseline ECG in these cases. Even if you feel fine, hidden risks like subclinical long QT syndrome can be detected this way. Don’t assume your doctor will order it; ask.
What are the warning signs of QT prolongation?
Symptoms can be subtle or sudden: dizziness, lightheadedness, palpitations (fluttering or pounding heart), fainting, or seizures. If you’re taking a macrolide and suddenly feel your heart racing or you pass out-even briefly-seek emergency care immediately. Torsades de pointes can progress to cardiac arrest within minutes.
Are there safer antibiotics for people with heart conditions?
Yes. For most common infections, alternatives like amoxicillin, doxycycline, cefdinir, or cephalexin carry no QT risk and are just as effective. For pneumonia, doxycycline is often preferred. For strep throat, penicillin remains the gold standard. Always ask your doctor: "Is there a non-macrolide option that works just as well?"
Can electrolyte imbalances make macrolide risks worse?
Absolutely. Low potassium (hypokalemia) and low magnesium double or triple the risk of TdP when combined with macrolides. Diuretics, laxatives, vomiting, or poor diet can cause these imbalances. If you’re on a water pill or have had recent illness with diarrhea or vomiting, get your electrolytes checked before taking a macrolide. Your doctor can order a simple blood test.
Is it safe to take azithromycin if I have a family history of sudden cardiac death?
Not without caution. Even if your ECG looks normal, a family history of unexplained sudden death under age 50 could signal an inherited long QT syndrome. These conditions often go undiagnosed until triggered by drugs like macrolides. Tell your doctor about this history. They may recommend genetic testing or avoid macrolides entirely in favor of safer alternatives.



Cassie Widders
January 12, 2026 AT 05:49Been on azithromycin twice for bronchitis and never thought twice about it. Guess I got lucky. My grandma had a bad reaction to something similar back in the 90s though-she just passed out in the kitchen and the ambulance barely made it in time. Never asked why. Should’ve asked more.
Darryl Perry
January 13, 2026 AT 21:46This post is accurate but overly alarmist. The absolute risk remains minuscule for the general population. Regulatory agencies don’t issue black box warnings lightly, but they also don’t ban these drugs because they’re lifesavers. Overmedicalization leads to unnecessary ECGs, increased costs, and patient anxiety. Don’t confuse statistical risk with clinical reality.
Konika Choudhury
January 14, 2026 AT 10:20USA and Europe overreact to everything. In India we give azithromycin like candy for fever and cough. Millions of doses every year. No mass cardiac collapse. Maybe your doctors are too scared to prescribe anything without 12 tests. We trust the medicine and the patient’s body. Your system is broken with too much fear and too little common sense.
Windie Wilson
January 14, 2026 AT 20:15So let me get this straight. The FDA says ‘maybe don’t give this to your 72-year-old grandma on diuretics and antidepressants’ and somehow that’s a scandal? Meanwhile, we’re still giving antibiotics for viral sinus infections like it’s 2003. The real problem isn’t QT prolongation-it’s that we treat every sniffle like a war zone. Also, I once got a 5-day azithromycin pack for a sore throat. I still have the pill bottle as a trophy.
Daniel Pate
January 15, 2026 AT 18:04It’s fascinating how we’ve turned medical risk into a quantifiable variable, yet still treat the human body as a black box. We measure QT intervals, track hERG blockade, and build risk calculators-but we ignore the fact that biology isn’t a spreadsheet. The real question isn’t whether azithromycin is dangerous-it’s why we still rely on blunt instruments like antibiotics when we have the tools to understand individual biology. Genetic screening, metabolic profiling, personalized dosing-these aren’t sci-fi. They’re just not profitable enough yet.
Amanda Eichstaedt
January 15, 2026 AT 18:47I’m a nurse in a rural clinic and I’ve seen this play out too many times. Old lady with CHF, on furosemide, takes azithromycin for a cough, ends up in the ER with TdP. Her doctor didn’t even check her meds list. We have the tools-ECG machines, MARC calculator, electrolyte panels-but we’re running on coffee and muscle memory. It’s not ignorance, it’s systemic exhaustion. Doctors aren’t villains. They’re drowning. We need better tech built into EHRs, not just another guideline nobody reads.
Ben Kono
January 16, 2026 AT 18:24My uncle died of sudden cardiac arrest at 58. No history. No symptoms. Just dropped dead while mowing the lawn. Turned out he had a hidden long QT mutation. They didn’t find it until after his autopsy. Now I ask every doctor if my meds will mess with my heart. No one ever says no. No one ever asks if I have family history. I’m not paranoid. I’m just tired of being a statistic
Jose Mecanico
January 17, 2026 AT 07:41Just wanted to add that if you’re on any diuretic, especially thiazides, check your potassium. Easy blood test. If it’s low, ask for a non-macrolide. It’s that simple. I’ve seen it save people.