What Exactly Is Metabolic Syndrome?
Metabolic syndrome isn’t a single disease. It’s a group of warning signs that show your body is struggling to manage energy properly. If you have three or more of these signs, your risk for heart disease, stroke, and type 2 diabetes jumps dramatically. The three biggest red flags? Your waist size, your triglyceride levels, and how well your body handles glucose.
It’s not about being overweight in general-it’s about where the fat sits. Carrying extra weight around your middle is the main trigger. That belly fat isn’t just storage; it’s active tissue that sends out harmful signals. These signals mess with how your body uses insulin, which then throws off your blood sugar and fats. It’s a cycle: more belly fat → worse insulin response → higher triglycerides → higher blood sugar → even more fat storage.
Why Your Waist Size Matters More Than Your Weight
Two people can weigh the same, but only one might have metabolic syndrome. The difference? Where the fat is. If you’re a man with a waist over 40 inches (102 cm), or a woman with a waist over 35 inches (88 cm), you’re in the danger zone according to U.S. guidelines. For South Asian, Middle Eastern, or some East Asian populations, the cutoff is even lower-around 31.5 inches (80 cm) for women and 37 inches (94 cm) for men.
Why does this matter? Belly fat releases chemicals that make your liver and muscles less sensitive to insulin. This isn’t just about looks. A 2018 study in Circulation found that every extra 4 inches (10 cm) around your waist raised heart disease risk by 10%, even after accounting for overall body weight. That’s why doctors now measure waist circumference as seriously as blood pressure.
Triglycerides: The Hidden Fat That’s Harming You
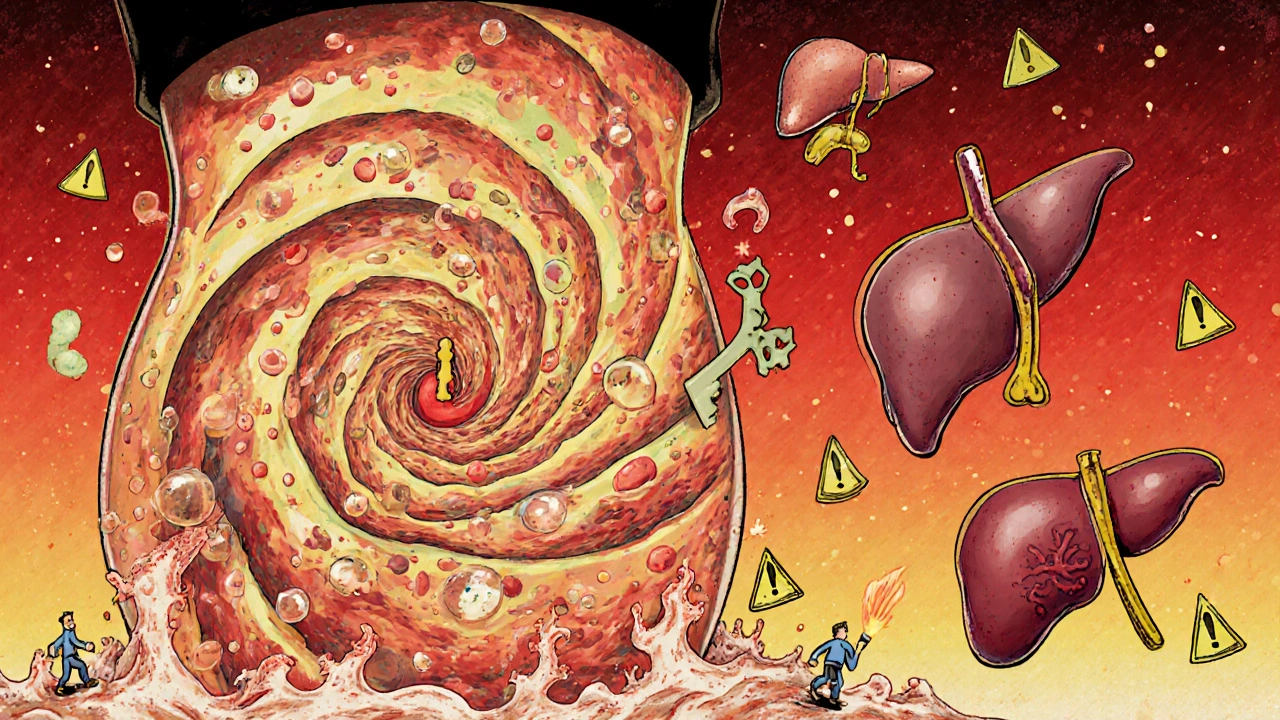
Triglycerides are the most common type of fat in your blood. Normal levels are below 150 mg/dL. If yours are 150 or higher, that’s one of the five signs of metabolic syndrome. But here’s the catch: levels above 200 mg/dL aren’t just a marker-they’re a direct threat. High triglycerides mean your liver is making too much fat and dumping it into your bloodstream as VLDL, a fatty particle that sticks to artery walls.
This isn’t just about diet. When insulin resistance kicks in, your body can’t store fat properly in muscle or fat cells. Instead, it shunts excess calories into the liver, which turns them into triglycerides. That’s why people with large waistlines almost always have high triglycerides. Even if your LDL (bad cholesterol) looks fine, high triglycerides still raise your risk of heart attack. The American Heart Association says levels over 200 mg/dL are considered high risk, regardless of other numbers.
Glucose Control: The Early Warning Before Diabetes
Your fasting blood sugar should be under 100 mg/dL. If it’s between 100 and 125 mg/dL, you have prediabetes-and you’re likely in the metabolic syndrome club. This isn’t a slow slide. Without change, 5% to 10% of people with prediabetes develop full-blown type 2 diabetes every year. That’s faster than most people realize.
The problem starts with insulin resistance. Your muscle and fat cells stop responding to insulin like they should. So your pancreas pumps out more insulin to compensate. Eventually, it burns out. Blood sugar rises. The body can’t move glucose into cells for energy, so it just sits in the blood, damaging blood vessels and nerves over time.
Here’s the link: high triglycerides make insulin resistance worse. Fat particles in the blood interfere with insulin’s ability to do its job. It’s a feedback loop-each problem feeds the other. That’s why fixing one often helps the others.
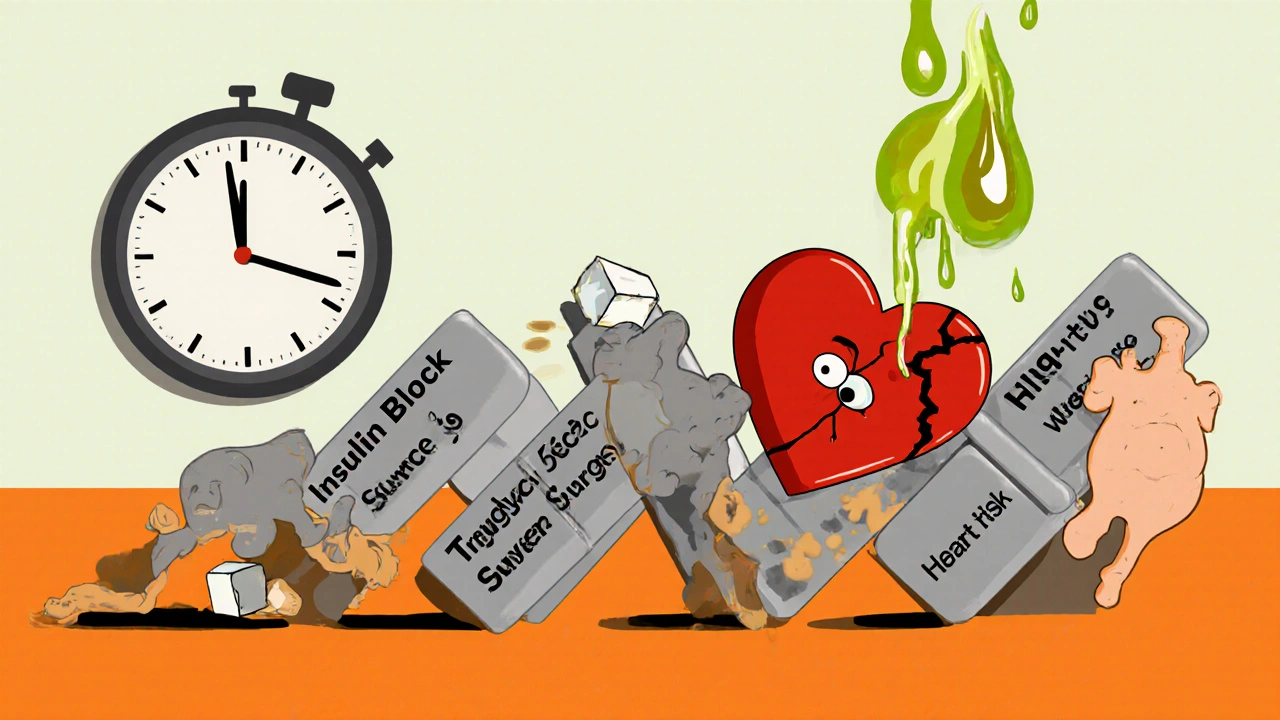
The Science Behind the Cycle: How It All Connects
Think of metabolic syndrome like a domino effect. It starts with too much belly fat. That fat releases inflammatory chemicals that block insulin signals. Without proper insulin function, your liver keeps making glucose even when you don’t need it. Your muscles can’t take in sugar, so blood glucose climbs.
At the same time, your liver starts turning extra carbs and fats into triglycerides. These flood into your blood. The more triglycerides you have, the more they interfere with insulin. The worse your insulin resistance gets, the more fat you store-especially around your belly. It’s a loop that gets harder to break the longer it runs.
Research from Washington University shows that this isn’t just theory. When people with metabolic syndrome had their fat tissue studied, they found high levels of harmful molecules like resistin and TNF-alpha-signs that fat cells are stressed and sending out damage signals. This is why losing even 5% of your body weight can reverse several of these markers at once.
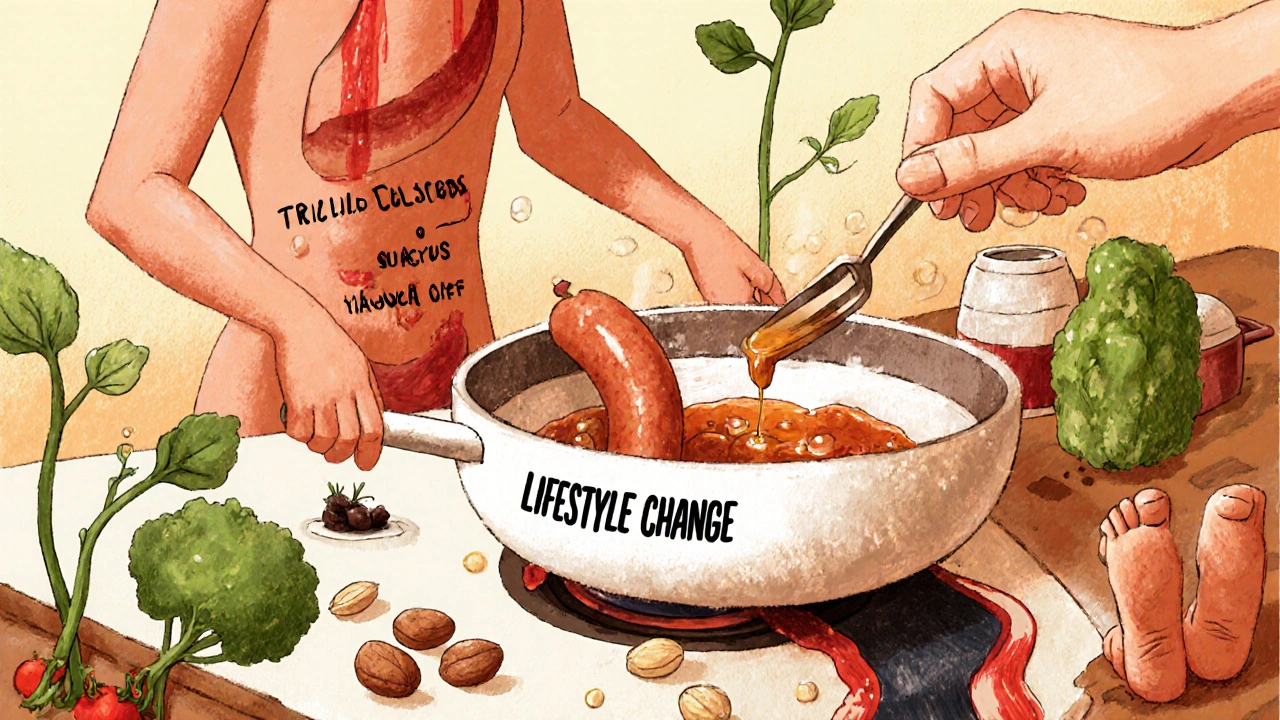
What You Can Do: Lifestyle Changes That Actually Work
Medication can help, but the only proven way to reverse metabolic syndrome is lifestyle change. And it’s not about extreme diets or punishing workouts. It’s about consistency.
- Move more: Aim for at least 150 minutes a week of brisk walking, cycling, or swimming. Studies show that even 30 minutes a day cuts waist size and improves insulin sensitivity.
- Change what you eat: Cut out sugary drinks, white bread, and processed snacks. Focus on vegetables, beans, whole grains, lean proteins, and healthy fats like olive oil and nuts. The PREDIMED trial found that people following a Mediterranean diet reduced heart events by 30%.
- Limit alcohol and sugar: Alcohol turns directly into triglycerides in the liver. The AHA recommends no more than two drinks a day for men, one for women. Added sugar? Keep it under 10% of your daily calories-that’s about 12 teaspoons for a 2,000-calorie diet.
- Sleep and stress matter: Poor sleep and high stress raise cortisol, which increases belly fat and blood sugar. Aim for 7-8 hours of sleep and find ways to manage stress-walking, breathing exercises, or time in nature.
Weight loss is the most powerful tool. Losing just 5-10% of your body weight can lower triglycerides by up to 40%, drop fasting glucose into the normal range, and shrink your waist significantly. You don’t need to lose 50 pounds. Start with 10.
When Medication Might Be Needed
Lifestyle is always first. But if your numbers are very high or you’ve already had a heart issue, your doctor might add medication. Metformin is often used to improve insulin sensitivity and lower blood sugar. Fibrates or prescription omega-3s can help bring down triglycerides if they’re above 500 mg/dL. Blood pressure meds like ACE inhibitors may be added if your pressure is consistently above 130/85.
But here’s the key: these drugs don’t fix the root problem. They manage symptoms. Only weight loss and better habits can reverse insulin resistance. Medication buys you time while you work on the deeper fix.
What’s Next: New Tools and Hope
Scientists are now looking beyond the standard five criteria. The triglyceride-glucose (TyG) index-calculated from your fasting triglyceride and glucose numbers-is showing promise as a simple way to spot insulin resistance early. Some labs now offer it as a routine test.
Research is also exploring the gut microbiome. People with metabolic syndrome have different gut bacteria than those without. Future treatments might include targeted probiotics or fiber supplements to rebalance these microbes.
And while global rates are rising-with WHO predicting half of adults in developed countries will have metabolic syndrome by 2030-the good news is this: it’s reversible. You don’t need a miracle. You need to start moving, eating better, and giving your body a chance to heal.
What to Ask Your Doctor
- What’s my waist measurement, and is it in the danger range?
- Are my triglycerides above 150? What’s my fasting glucose?
- Do I have insulin resistance? Is there a test for that?
- Should I get checked for prediabetes or early heart disease?
- Can we create a plan that focuses on losing 5-10% of my weight first?
Metabolic syndrome isn’t a life sentence. It’s a signal. Your body is telling you something’s off. Listen. Start small. Focus on your waist, your fats, and your blood sugar-and you can turn it all around.



Vanessa Carpenter
November 27, 2025 AT 07:49So many people think it’s all about the scale, but honestly? My waist shrunk before the scale even moved after I started walking daily. It’s wild how much just moving more changes your body’s chemistry. No crazy diets, no supplements-just consistency.
And yeah, the belly fat thing? It’s real. I used to joke about my ‘dad bod’ until I got my numbers checked. Now I’m just trying to outsmart my own biology.
Michael Collier
November 28, 2025 AT 15:11It is imperative to underscore that metabolic syndrome constitutes a constellation of interrelated physiological derangements, the pathophysiological nexus of which is visceral adiposity-induced insulin resistance. The adipose tissue, particularly in the abdominal region, functions not merely as an energy reservoir but as an endocrine organ secreting adipokines such as resistin and tumor necrosis factor-alpha, which directly impair insulin signaling cascades.
Consequently, hepatic gluconeogenesis is upregulated, peripheral glucose uptake is diminished, and de novo lipogenesis is accelerated, culminating in hypertriglyceridemia and hyperglycemia. The clinical imperative, therefore, is not pharmacological suppression of individual biomarkers, but the restoration of metabolic homeostasis through sustained lifestyle intervention.
Shannon Amos
November 30, 2025 AT 14:22So let me get this straight-we’re supposed to believe that eating a salad and walking around the block is going to undo 20 years of pizza and Netflix? Cool. I’ll just add ‘reverse metabolic syndrome’ to my to-do list next to ‘learn to meditate’ and ‘stop procrastinating.’
Also, who decided waist size was more important than BMI? Did they just pick a number out of a hat? 😏
Ginger Henderson
November 30, 2025 AT 16:42Yeah but what if you’re just naturally big-boned? My grandma had a 38-inch waist and lived to 92. She never ate kale. Maybe the whole thing’s just fear-mongering dressed up as science.
Bethany Buckley
December 2, 2025 AT 03:13Interestingly, the TyG index (log[triglycerides × glucose]/2) demonstrates superior predictive validity for insulin resistance compared to traditional diagnostic criteria, as evidenced by recent longitudinal cohort analyses (e.g., Kim et al., 2022, *Diabetologia*). Moreover, the gut microbiome’s role in SCFA production-particularly butyrate-mediated GPR43 activation-modulates adipose inflammation and insulin sensitivity via epigenetic pathways. The reductionist framing of ‘lose weight, eat better’ ignores the emergent complexity of metabolic dysregulation at the systems biology level.
Also, 🌱✨
Cynthia Boen
December 3, 2025 AT 23:08This article is just another guilt trip wrapped in medical jargon. You think I don’t know I’m supposed to ‘eat better’? I’ve read every damn article. The real issue is that no one gives a damn about food deserts, or how stress from working two jobs makes you crave sugar. Stop blaming individuals and fix the system.
Amanda Meyer
December 5, 2025 AT 14:56I appreciate the depth here, but I’m curious-how much of this is influenced by genetics versus environment? I have a family history of diabetes and high triglycerides, yet I’ve maintained a healthy waist and active lifestyle. Is it possible to be ‘metabolically healthy obese’? Or is that just a myth?
Jesús Vásquez pino
December 7, 2025 AT 00:54Okay but I’ve been doing all this-walking, eating clean, sleeping well-and my triglycerides are still 210. What am I missing? Am I just doomed? Also, why does everyone act like weight loss is the only answer? I’m not trying to be skinny, I just want to not feel like I’m one heart attack away from death.
vikas kumar
December 7, 2025 AT 20:16In India, we see this a lot-people with normal BMI but high waist circumference because of sedentary jobs and lots of refined carbs like white rice and fried snacks. The cutoffs for South Asians? Spot on. My uncle had all the markers, lost 12 pounds, and his triglycerides dropped 60% in 4 months. No meds. Just food changes and walking after dinner. Small steps, big results.
Bea Rose
December 9, 2025 AT 02:41stephen riyo
December 10, 2025 AT 09:58Wait-so if I lose 10% of my weight, my triglycerides drop 40%? That’s… actually kind of amazing? I’ve been avoiding this article because I thought it was going to be another ‘you’re lazy’ lecture, but this actually gave me hope. I’m gonna start with just walking after dinner. No pressure. Just… one step. Maybe I can do this.