Metformin Lactic Acidosis Risk Assessment
This assessment helps you understand your personal risk of lactic acidosis while taking metformin. Based on FDA data, lactic acidosis occurs in less than 1 in 10,000 metformin users, but it can be life-threatening when it happens. Select the conditions that apply to you to get your personalized risk assessment.
Your Risk Factors
Select all conditions that apply to you. These factors can increase your risk of lactic acidosis.
Risk Assessment Results
Important Warning
If you have any of these risk factors, especially kidney issues or alcohol use, you should talk to your doctor before taking metformin or if you're already on it.
Key Warning Signs
If you experience any of these symptoms while taking metformin, seek emergency medical attention immediately:
- Extreme tiredness or weakness
- Rapid, shallow breathing
- Unexplained nausea or vomiting
- Deep stomach pain
- Muscle aches or cramps without reason
- Feeling unusually cold
These symptoms appear in 95% of lactic acidosis cases and require immediate medical attention.
Metformin is the most prescribed diabetes medication in the world. Millions of people take it daily to control blood sugar, and for most, it works well with few problems. But not everyone tolerates it. Two risks stand out: uncomfortable stomach issues and a rare but dangerous condition called lactic acidosis. If you’re on metformin-or thinking about starting it-you need to know what’s normal, what’s serious, and what to do next.
Why Metformin Causes Stomach Problems
About 1 in 3 people who start metformin get gastrointestinal side effects. That’s not rare-it’s expected. Diarrhea is the most common, hitting over half of those affected. Nausea, stomach cramps, vomiting, and loss of appetite follow close behind. These aren’t allergies. They’re direct reactions to how the drug works in your gut.
Metformin doesn’t get absorbed quickly. Instead, it sits in your intestines, changing how gut bacteria behave and irritating the lining. That’s why symptoms usually show up in the first week or two. A 1998 UK study found that nearly 7 out of 10 people felt something within 30 days of starting the pill.
Here’s the good news: most of these symptoms fade. About 85% of people see major improvement within 2 to 4 weeks. You’re not stuck with them. The key is patience and smart dosing.
How to Reduce GI Side Effects
There’s no magic trick, but proven strategies work. The first is switching to the extended-release version. Metformin ER releases the drug slowly, so less of it hits your gut all at once. A 2023 review of patient reports showed that 78% of people who switched from regular metformin to ER saw their diarrhea drop from daily episodes to occasional mild cramps.
Start low. Many doctors still prescribe 500 mg twice a day right away. That’s too fast. Start with 500 mg once a day, preferably with your evening meal. After a week, if you feel okay, bump it to 500 mg twice a day. Wait another week before going higher. This slow ramp-up cuts side effects in half.
Take it with food. Always. Even if you’re not hungry. Food slows absorption and reduces irritation. Skip the empty-stomach habit-it’s a recipe for nausea.
Hydrate. Diarrhea drains fluids and electrolytes. Drink water regularly. Don’t wait until you’re thirsty. Coconut water or low-sugar electrolyte drinks help if you’re losing a lot.
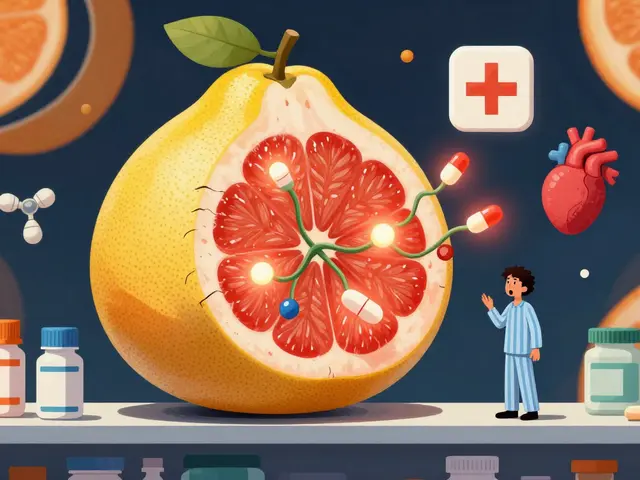
Lactic Acidosis: The Rare but Deadly Risk
Lactic acidosis sounds scary-and it is. But it’s extremely rare. Studies estimate only 1 to 9 cases per 100,000 people taking metformin each year. That’s less than 1 in 10,000. For comparison, you’re more likely to be struck by lightning.
But when it happens, it’s dangerous. About 30 to 50% of people who develop metformin-associated lactic acidosis (MALA) die from it. That’s why it carries a black box warning from the FDA-the strongest safety alert they have.
Here’s what you need to know: MALA doesn’t happen in healthy people on the right dose. It happens when your body can’t clear metformin or lactate. That usually means one or more of these:
- Severe kidney problems (eGFR below 30)
- Acute kidney injury from infection, dehydration, or shock
- Liver failure
- Heart failure
- Excessive alcohol use
- Age over 80 with other health issues
Metformin doesn’t cause lactic acidosis in healthy kidneys. It just makes it harder for your body to clear lactate if you’re already sick. Think of it like a clogged drain. The drug doesn’t create the clog-it just makes it worse if the pipe was already blocked.
Warning Signs You Can’t Ignore
If you’re on metformin, learn these symptoms. Don’t wait. Call your doctor or go to the ER immediately if you have:
- Extreme tiredness or weakness-so bad you can’t get out of bed
- Rapid, shallow breathing (not from exercise or anxiety)
- Unexplained nausea or vomiting that won’t stop
- Stomach pain that feels deeper than normal cramps
- Muscle aches or cramps without reason
- Feeling unusually cold, especially in your arms and legs
These aren’t guesses. Data from over 1,200 confirmed MALA cases show these symptoms appear in nearly all cases. Fatigue shows up in 95% of them. Rapid breathing? 88%. These are red flags, not side effects.
Doctors confirm MALA with blood tests: arterial pH below 7.35, lactate levels above 5 mmol/L, and an anion gap over 12. If you’re in the hospital and your bloodwork shows this, they’ll stop metformin immediately and start aggressive treatment-fluids, bicarbonate, dialysis.

Who Should Not Take Metformin
Metformin isn’t for everyone. Absolute contraindications are clear:
- eGFR below 30 mL/min/1.73m² (severe kidney disease)
- Acute kidney injury
- Severe liver disease
- Heart failure requiring hospitalization
- Alcoholism or heavy drinking (3+ drinks daily)
- History of lactic acidosis
Also, if you’re getting a CT scan or angiogram with contrast dye, you must stop metformin 48 hours before and wait 48 hours after. Contrast can stress your kidneys. If they’re already borderline, metformin can push you into danger.
Don’t assume your doctor already knows your full history. Tell them about every condition, every medication, every drink you have. Even if you think it’s not relevant.
Metformin and Kidney Damage: A Myth
Many people think metformin harms the kidneys. It doesn’t. A 10-year study tracking 12,000 users found no increased risk of kidney damage. In fact, metformin may protect kidney function in early-stage diabetes.
What happens is the opposite: if your kidneys are already failing, metformin builds up. That’s why we check kidney function before and during treatment. The drug isn’t the cause-it’s a warning sign that your kidneys need help.
Doctors now monitor eGFR every 3 to 6 months if your kidney function is between 45 and 59. If it drops below 45, they check monthly. If it hits 30 or lower, they stop metformin. That’s not because the drug is toxic-it’s because your body can’t handle it anymore.
What’s New in Metformin
In May 2023, the FDA approved a new extended-release formula called Metformin-ER-XR. In clinical trials, it caused 43% fewer stomach problems than older versions. That’s a big deal for people who had to quit metformin before.
Another exciting area is the TAME trial-Targeting Aging with Metformin. Funded by the NIH with $72 million, it’s testing if metformin can delay aging-related diseases. But don’t rush to take it for longevity. There’s no proof yet, and the American Federation for Aging Research warns against off-label use.

What About Vitamin B12?
Yes, long-term metformin use can lower B12 levels. About 7% of people on it for more than 4 years see a drop. But it’s usually mild and reversible. A 2022 study found that 94% of people who took B12 supplements returned to normal levels.
That’s why the American Association of Clinical Endocrinologists now recommends checking B12 every year if you’ve been on metformin for more than 3 years. If your levels are low, a simple over-the-counter supplement fixes it. No need to stop the diabetes drug.
Final Thoughts: Is Metformin Still Safe?
In 2022, the FDA reviewed 15.2 million metformin users. Only 12 confirmed cases of lactic acidosis were found. That’s 0.079 cases per 100,000 people. The risk is lower than being hit by a car while crossing the street.
Metformin is safe when used correctly. The real danger isn’t the drug-it’s ignoring your body’s signals or skipping kidney checks. If you have kidney disease, liver problems, or drink heavily, talk to your doctor before starting. If you’re already on it and feel unwell, don’t assume it’s just stomach upset. Listen to your body.
For most people, metformin is the best tool they have to manage type 2 diabetes. It’s cheap, effective, and helps with weight. The side effects? Usually temporary. The risks? Rare and preventable. You don’t need to fear it. You just need to know how to use it wisely.
Can metformin cause permanent stomach damage?
No. Metformin doesn’t cause lasting damage to your stomach or intestines. The gastrointestinal side effects-like diarrhea and nausea-are temporary and usually resolve within 2 to 4 weeks. If symptoms persist beyond that, it’s likely due to another cause, like an infection or food intolerance. Switching to an extended-release form or adjusting the dose often resolves the issue completely.
Is lactic acidosis common with metformin?
No, it’s extremely rare. Studies show only 1 to 9 cases per 100,000 people taking metformin each year. The FDA’s 2022 review of 15.2 million users found just 12 confirmed cases. Most cases occur in people with severe kidney disease, liver failure, or other serious illnesses. If your kidneys are working normally and you don’t drink heavily, your risk is virtually zero.
Should I stop metformin if I get diarrhea?
Not immediately. Diarrhea is common in the first few weeks and usually goes away on its own. Try taking the extended-release version, reduce your dose, and take it with food. If it lasts longer than 4 weeks, gets worse, or you become dehydrated, talk to your doctor. Never stop metformin without medical advice-uncontrolled blood sugar is far more dangerous than temporary stomach upset.
Can I take metformin if I have mild kidney issues?
Yes, if your eGFR is between 30 and 45, you can still take metformin, but your doctor will monitor you more closely. They’ll check your kidney function every month. If your eGFR drops below 30, they’ll stop the medication. Many people with early-stage kidney disease benefit from metformin’s blood sugar control and weight benefits-just with extra caution.
Does metformin cause weight loss?
Yes, modestly. On average, people lose 2 to 4 kilograms (4 to 9 pounds) in the first year. It’s not a weight-loss drug, but it helps reduce appetite and improves how your body uses insulin. This makes it ideal for people with type 2 diabetes who are overweight. Unlike some other diabetes meds, it doesn’t cause weight gain.
Can I drink alcohol while taking metformin?
Occasional moderate drinking (1 drink per day for women, 2 for men) is usually safe. But heavy or binge drinking increases your risk of lactic acidosis. Alcohol affects your liver and kidneys, which are already working to clear metformin. If you drink regularly, tell your doctor. They may adjust your dose or monitor you more closely.
What to Do Next
If you’re on metformin:
- Check your kidney function every 3 to 6 months (or monthly if eGFR is below 45).
- Ask your doctor about switching to extended-release if you have stomach issues.
- Get your vitamin B12 checked yearly if you’ve been on metformin for more than 3 years.
- Stop metformin 48 hours before any imaging test with contrast dye.
- Know the warning signs of lactic acidosis and act fast if you feel them.
If you’re thinking about starting metformin:
- Ask for a kidney function test before you begin.
- Request the extended-release version from the start-it’s easier on your stomach.
- Start with the lowest dose and increase slowly.
- Take it with food, every time.
Metformin has been helping people manage diabetes for over 65 years. It’s not perfect, but it’s one of the safest, most effective drugs we have. The key isn’t avoiding it-it’s using it the right way.




vivek kumar
January 17, 2026 AT 18:56Metformin’s GI side effects are overblown. I started at 500mg twice daily with no ramp-up, and within 10 days, my diarrhea vanished. The real issue is doctors who treat patients like lab rats instead of humans. Slow titration isn’t optional-it’s basic pharmacology. If your doc pushes you straight to 1000mg, find a new one.
waneta rozwan
January 18, 2026 AT 17:45Let me just say this: if you’re taking metformin and you’re not terrified of lactic acidosis, you’re not paying attention. I had a cousin who thought ‘rare’ meant ‘impossible’-ended up in the ICU with a pH of 6.9. They had to dialyze him for three days. This isn’t ‘oh I got a tummy ache’-this is death by a thousand cuts you didn’t see coming. Read the black box warning. Actually read it. Not just skim it while scrolling TikTok.
john Mccoskey
January 20, 2026 AT 03:30There’s a fundamental cognitive dissonance in how the medical community frames metformin risk. On one hand, they tout it as ‘safe and effective’-a first-line wonder drug. On the other, they slap on a black box warning that screams ‘this can kill you.’ The truth? It’s neither. It’s a tool with narrow therapeutic boundaries. The danger isn’t the molecule-it’s the systemic failure to individualize dosing based on renal function, comorbidities, and alcohol use. We treat diabetes like a spreadsheet, not a living physiology. And that’s why people die. Not because metformin is evil-but because medicine has outsourced judgment to algorithms and guidelines that ignore context.
Joie Cregin
January 21, 2026 AT 02:17My grandma’s been on metformin for 12 years and still hikes every morning. She takes ER, eats her dinner with it, and checks her B12 yearly like clockwork. She doesn’t panic about lactic acidosis-she just lives smart. If you’re healthy, your kidneys work, and you don’t chug whiskey like it’s water? You’re probably fine. The fear-mongering online is louder than the science. Take the pill. Take it with food. Get your labs done. Breathe. You got this.
Melodie Lesesne
January 22, 2026 AT 09:19Switched to ER last year after 3 weeks of nonstop diarrhea. Game changer. I didn’t even realize how bad it was until it stopped. Now I just take it with my bedtime snack and forget about it. Also got my B12 checked-was low, started a $5 supplement, and my brain fog cleared. Metformin’s not perfect, but it’s been a lifesaver for my blood sugar. Just listen to your body and don’t be shy about asking for ER.
brooke wright
January 22, 2026 AT 14:33Wait-so if I have mild kidney issues and take metformin, I’m basically playing Russian roulette with my liver? And you’re telling me to just ‘monitor’? What if my doctor forgets? What if I miss a blood test? How many people die quietly because no one checked their eGFR that month? This isn’t a lifestyle tweak-it’s a minefield.
Kasey Summerer
January 24, 2026 AT 10:28So let me get this straight: a drug that causes diarrhea in 1 in 3 people, has a black box warning, and requires you to stop it before every CT scan… is the ‘best tool we have’? Bro, if this is the gold standard, the bar is in the basement. I’d rather eat sugar and take insulin than risk becoming a statistic in a 2024 medical journal. 🤷♂️
kanchan tiwari
January 25, 2026 AT 17:01Metformin is a government plot to control the diabetic population. The FDA approved it because Big Pharma owns the WHO. They want you dependent on pills so you’ll keep coming back for more tests, more meds, more dialysis. Lactic acidosis? That’s just the cover story. The real goal is to keep you sick and billing insurance. Don’t be fooled. Try fasting. Try berberine. Try asking questions. They don’t want you to.